An optometrist's role in concussion
Concussion and mild traumatic brain injury have received more media and literature attention in recent years and our understanding of these conditions is increasing. Optometrists are perfectly placed to help those individuals with concussion and often simple changes can make enormous differences to the lives of people who have suffered any neurological event.
Post-trauma vision syndrome (PTVS) was first coined in the mid-90s by Bill Padula who recognised many people who suffer a traumatic brain injury (TBI) will present with a characteristic set of clinical findings. These include exotropia or high exophoria, convergence insufficiency, accommodative issues, low blink rate, spatial disorientation, poor fixations, poor pursuits and unstable ambient vision. PTVS may also affect gait, posture and musculoskeletal presentation.
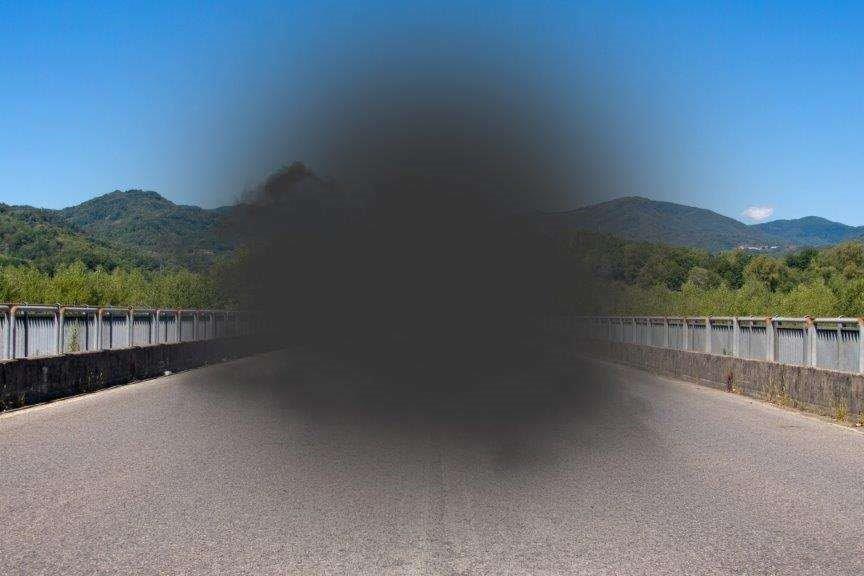
Recent literature has also shown a significant proportion of mild traumatic brain injury (mTBI) sufferers experience visual issues, especially relating to the oculomotor system and accommodative and vergence deficits¹,². The prevalence of visual midline shift syndrome (VMSS) after TBI has also recently been estimated to be very high³.
Examination of a patient with PTVS often requires more time and empathy during assessment and it may be necessary to spread the assessment over more than one visit. Examination should include most of the procedures used in a standard assessment, as well as additional procedures aimed at probing performance. Refractive changes after a mild TBI have been well documented with a myopic shift being more likely⁴,5,6. Subjective binocular and monocular accommodation measurement should be attempted and repeated. It is not uncommon for this population to have near-to-normal initial findings then, as the patient fatigues, to find the repeat measurements significantly reduced. Similarly, near point of convergence (NPC) should be repeated, especially as reduced NPC is one of the most prevalent findings after TBI.
Use of the King-Devick Test to assess saccadic function has also recently received attention, both in New Zealand and overseas, and its efficacy in assessing concussion on the sidelines of sporting events is promising⁷,⁸. The possibility of VMSS should not be overlooked and, although assessment initially requires a little experience, it is relatively easy to perform.
Visual field assessment should always be attempted with test pauses whenever necessary to re-establish concentration, a common issue post-TBI. Visual field loss can take many forms on account of the susceptibility of the visual pathway to insult.
In prescribing, a general rule is to avoid multifocal lenses whenever possible and never to underestimate the benefit of small prescriptions and the use of small amounts of base-in prism at near. Treatment with tinted lenses should also be considered, though care needs to be taken in prescribing. Careful titration of tint has been considered for many years⁹ and this opinion has gained more traction recently¹⁰,¹¹.
The use of yoked prism in TBI is invaluable due to the effect the prism can have on the ambient visual system and the benefit this can give to a patient with VMSS. Similarly, the effectiveness of binasal occlusion has been studied and compared favourably with the benefits of base-in prism¹². Recent literature has also discussed why so many optometrists find this treatment to be so effective¹³,¹⁴.
Vision therapy can provide significant relief in this population, especially those with accommodation and vergence issues. The gold standard CITT study has shown that the best treatment for convergence insufficiency is in-office vision therapy¹⁵.
For optometrists interested in learning more about this worthwhile and thought-provoking field, regular courses are available through ACBO (the Australasian College of Behavioural Optometrists, the College of Optometrists in Vision Development and NORA (the Neuro-Optometric Rehabilitation Association). New Zealand also has a small but vibrant group of professionals who correspond regularly to discuss examination, treatment and case records of patients from this population.
References
1. K. Ciuffreda, "Occurence of Oculomotor Dysfunctions in Acquired Brain Injury; A Retrospective Analysis," Optometry, vol. 78, pp. 155-161, 2008.
2. G. L. Goodrich, J. Kirby, G. Cockerham, S. P. Ingalla and H. L. Lew, "Visual Function in Patients of a Polytrauma Rehabilitation Centre," Journal of Rehabilitation Research and Development, vol. 44, no. 7, pp. 929-936, 2007.
3. D. Tong, J. Cao, A. Beaudry and E. Lin, "High Prevalence of Visual Midline Shift Syndrome in TBI," Vision Dev & Rehab, vol. 2, no. 3, pp. 176-84, 2016.
4. B. J. Bohlmann and T. D. France, "Persistent Accommodative Spasm Nine Years After Head Trauma," J Clin Neuroophthalmol, vol. 7, no. 3, pp. 129-34, 1987.
5. M. L. Monteiro et al, "Persistent Accommodative Spasm After Severe Head Trauma," Br J Ophthalmol, vol. 87, no. 2, pp. 243-4, 2003.
6. F.E. Hughes et al, "Persistent Pseudomyopia Following a Whiplash Injury in a Previously Emmetropic Woman," Am J Ophthalmol Case Rep, vol. 22, no. 8, pp. 28-30, 2017.
7. D. King et al, "Use of the King-Devick Test for Sideline Concussion Screening in Junior Rugby League," Journal of Neurological Sciences, vol. 357, no. 1-2, pp. 75-79, 2015.
8. J. P. MacDonald et al, "Reliability of the King-Devick Test in Baseline Concussion Evaluations of High School Athletes," Medicine and Science in Sports and Exercise, vol. 48, no. 5S, pp. 627-628, 2016.
9. J. Lebensohn, "The Nature of Photophobia," Arch Ophthalmol, vol. 12, pp. 380-3, 1934.
10. J. Q. Truong, K. J. Ciuffreda, M. H. Han and I. B. Suchoff, "Photosensitivity in Mild Traumatic Brain Injury (mTBI)," Brain Injury, vol. 28, no. 10, pp. 1283-7, 2014.
11. Y. Wu and M. Hallett, "Photophobia in Neurological Disorders," Translational Neurodegeneration, vol. 6, p. 26, 2017.
12. N. K. Yadav and K. J. Ciuffreda, "Effect of Binasal Occlusion and Base-In Prisms on the Visual Evoked Potential in Mild Traumatic Brauin Injury (mTBI)," Brain Inj, vol. 28, no. 12, pp. 1568-80, 2014.
13. S. Gallop, "Binasal Occlusion - Immediate Sustainable Relief," Optom Vis Perform, vol. 2, no. 2, pp. 74-78, 2014.
14. A. Proctor, "Traumatic Brain Injury and Binasal Occlusion," Optom Vis Dec, vol. 40, no. 1, pp. 45-50, 2009.
15. M. Scheiman et al, "A Randomised Clinical Trial of Treatments for Convergence Insufficiency in Children," Arch Ophthalmol, vol. 123, pp. 14-24, 2005.
Niall McCormack is optometrist director of Specsavers Hastings, an honorary academic at Auckland University and a volunteer for the Fred Hollows Foundation and Eye Care for Africa. He has a particular interest in paediatric eye health and neuro-optometry.