APAO 2019: The sciences and arts of ophthalmology
The Asia Pacific Academy of Ophthalmology’s 34th Congress was held in the beautiful city of Bangkok, against a backdrop of gorgeous temples juxtaposed with modern architecture mirroring this year’s APAO theme of the sciences and arts of ophthalmology.
The four-day conference was jam-packed with more than 5000 delegates all eager to participate in some of the hundreds of rapid-fire sessions, symposia, plenary sessions, poster presentations and multiple social occasions. With such a full week of learning, networking, connecting with friends and colleagues as well as eating delicious Thai food there is almost too much to comment on. However, as I reviewed the copious notes and photos I’d taken, I noted there were three main areas which I kept returning to as my highlights from this year’s APAO conference: a large interdisciplinary panel discussion about the overlap of glaucoma and myopia, the rise and implementation of artificial intelligence (AI) in eye care and New Zealand’s large contribution to APAO 2019.
Myopia and glaucoma
The interdisciplinary panel brought together to discuss the association between myopia and glaucoma were asked and attempted to answer the question, ‘We often talk about myopia and glaucoma being associated, but what does the current research tell us and what should we be advising patients in clinical practice?’
The association of glaucoma and myopia has been recognised for many years with an increasing association with high (over -8DS) and very high (over -12DS) myopes. However, current literature, including the famous ocular hypertension study, indicates myopia is not an independent risk factor for conversion of ocular hypertension to glaucoma. It’s also been shown that myopia is not a risk factor for glaucoma progression in individuals with early glaucoma. Therefore, the presence of myopia does not indicate that a patient’s glaucoma will progress more than those without myopia.
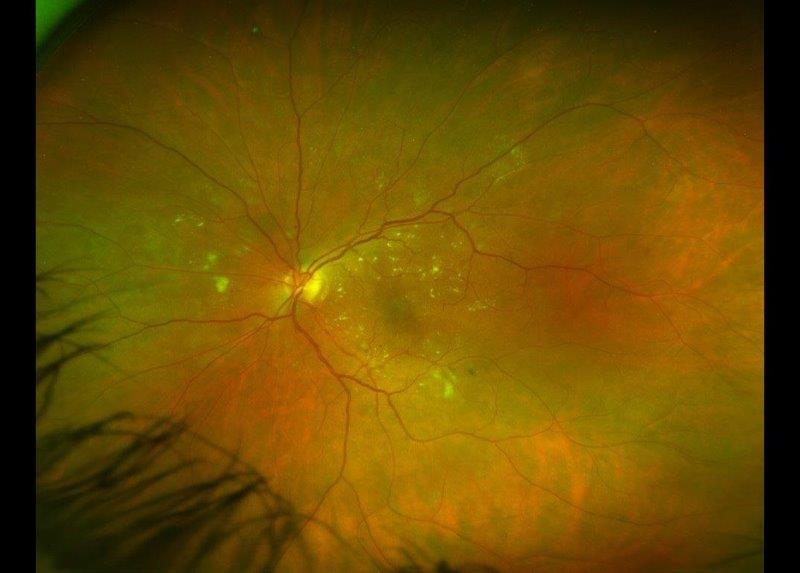
The discussion then turned to the challenge of diagnosing glaucoma in myopes. Individuals with myopia can have variable appearances of their optic nerves making aspects hard to assess or measure, large areas of peripapillary atrophy and myopic visual field loss that can appear similar to a glaucomatous visual field.
As both conditions have similar clinical signs, this has led to research to determine if there is a shared mechanism in myopia and glaucoma development. Current research, however, supports an association between myopia and glaucoma but not a causal relationship.
Optical coherence tomography (OCT) of the optic nerve has become a key aspect of glaucoma diagnosis, however, due to the variation in appearance of myopic nerves the results can be highly variable. Many panellists called for the development of a myopic normative OCT dataset to help with the diagnosis of glaucoma in these challenging cases.
A clinical pearl suggested was to use vertical macula scans to compare the differences in superior to inferior ganglion cell density. The comparison of superior and inferior portions aligns with glaucoma’s adherence to the horizontal midline. However, the key point that continued to be made was that although glaucoma diagnosis can be extremely challenging in eyes with myopia the main difference is that glaucoma is a progressive disease. Thus, the panellists reminded the audience that individuals with myopia who you suspect have glaucoma should be watched closely for progression with intervention not recommended until progression can be documented.
AI and ophthalmology
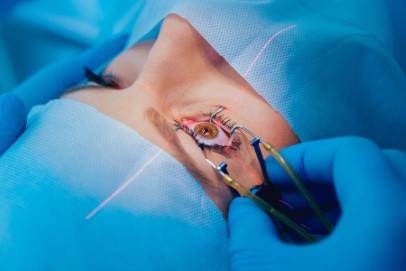
Another aspect of APAO that grabbed my attention was the many presentations and discussions about AI. Research has been exploding in the AI area and its potential application for ophthalmology. The vast array of data, however, with its high level of complex technological aspects can be hard to comprehend.
It was emphasised by many that accurate AI research should always report the total number of patients, number of eyes and the number of images used separately, and it should have an appropriate design validation. Effective AI design requires a developmental set of images - a set for primary clinical internal validation and a secondary set for clinical data assessment. The images used need to be of high quality as the information put into an AI system will determine the reliability of the information coming out. Information used to ‘train’ an AI system should vary in aspects such as contrast, brightness, flip and rotation to increase the robustness of the AI development algorithm and thus the accuracy of the data the AI system produces. This helps to ensure the AI system is detecting the disease and not just similarities in images due to how those images were captured.
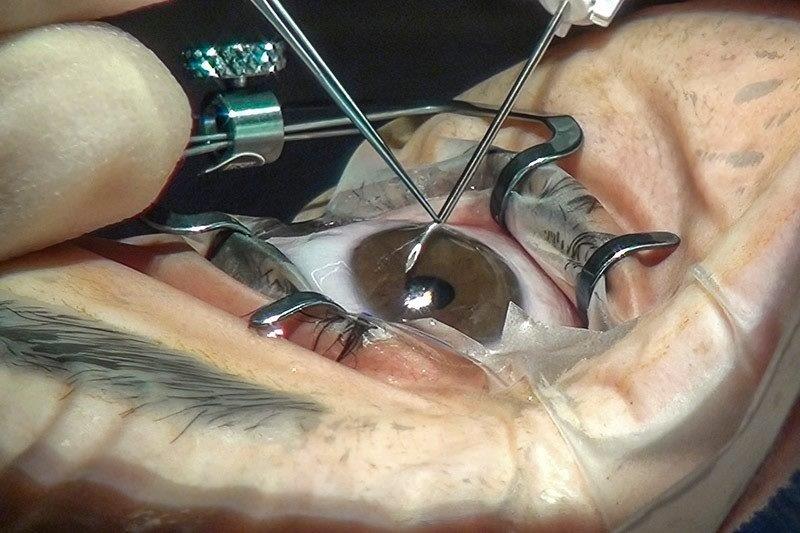
AI has been researched primarily in diabetic retinopathy with subsequent developments in retinopathy of prematurity (ROP), glaucoma and age-related macular degeneration. Professor Michael Chiang Knowles, professor of ophthalmology and medical informatics and clinical epidemiology at Oregon Health and Science University, is known for his AI work in collaboration with Google. He observed the significant difference in ophthalmologists diagnosing plus disease in ROP, a key component in the decision to treat. The AI algorithm he developed focused on putting a quantitative score on the qualitative assessment of plus in ROP to change the subjective opinion of ‘it just looks bad’ to a quantitative value to try and reduce the variance between conservative and aggressive ROP treaters.
The future of AI isn’t as simple as finding the right images to feed into a computer. Many questions remain including: who is responsible if the computer makes an incorrect diagnosis? Will doctors lose their jobs? How can machines do a better job than us in detecting highly varying diseases? Although many questions remain, AI appears to be here to stay, so we must continue to learn and develop alongside it.
New Zealand at APAO
I found the 2019 APAO conference a special year to attend as it was New Zealand Professor Charles McGhee’s final year as president. He finished his tenure on a high note chairing four sessions, giving seven presentations and presenting at multiple awards and social events. Charles spear-headed the 2019 APAO conference and development of the society during his time as president and he is a wonderful reminder of the huge contribution our small nation makes to the international world of ophthalmology.
Charles’ leadership in New Zealand was highlighted by the number of researchers presenting a wide variety of work from the University of Auckland’s Department of Ophthalmology. This included but was not limited to: Joyce Mathan with a poster on her pilot work assessing the prevalence of keratoconus in Down syndrome; Dr Akilesh Gokul presentation on the importance of understanding corneal biomechanics and Dr Jie Zhang’s talk about her wonderful work on the corneal endothelium. While Dr Jina Han shared some interesting cases on accidental and surgical trauma to the eye and I was honoured to give a presentation on the rising occurrence of cerebral visual impairment and the morphological development of the optic nerve in children born prematurely.
To walk around at one of the largest ophthalmology conferences in the world and hear Kiwi accents and see many friends and colleagues from our home so far away, brings an amazing amount of pride as well as an assurance that we are providing the most up-to-date eye health knowledge we can to our patients back in New Zealand.
In conclusion
Our trip to Thailand was fast and vast with lots eaten, lots learnt, and lots to think about. APAO 2019 was a roaring success and I look forward to the next APAO in Xiamen, China from 22-26 April 2020 with baited breath to hear updates on all that was new at this year’s APAO and proudly see the role little old New Zealand continues to play.
Dr Samantha Simkin is a therapeutically-qualified optometrist, a member of the BLENNZ National Assessment Team and the Stevenson post-doctoral research fellow at the University of Auckland.