Assessing retinal damage from anti-VEGF injections
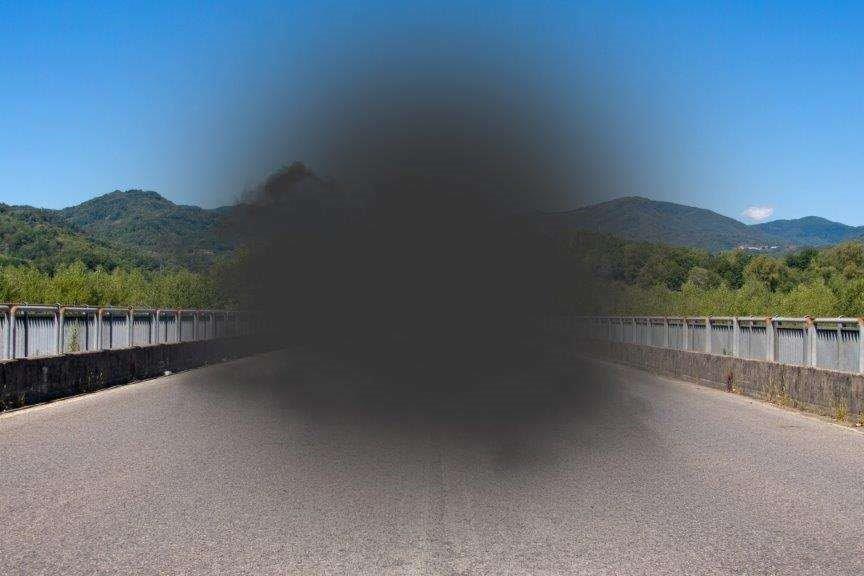
In a first of its kind study, Mount Sinai Hospital researchers used optical coherence tomography angiography (OCTA) to measure potential retina damage from long-term use of intravitreal eye injections. The findings suggest repeated use of these injections could contribute to progressive vision loss after many years, paving the way for new treatment approaches to mitigate the problem.
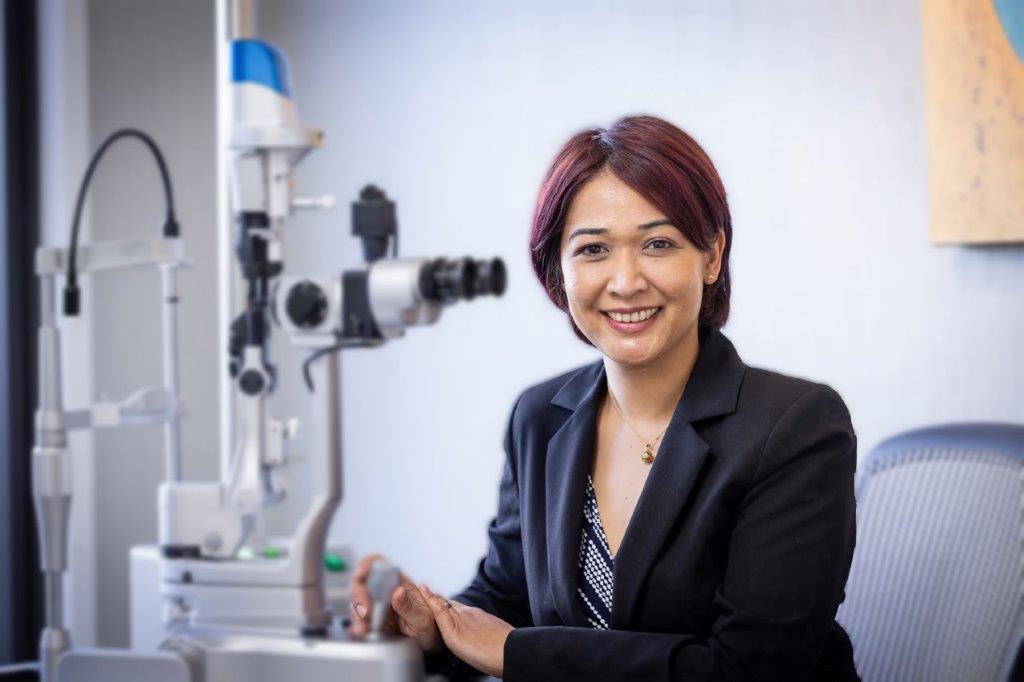
With intravitreal injections being relatively new, the study was prompted by a wish to understand the long-term effects of anti-VEGF injections in the eye, said senior investigator Professor Richard Rosen from the Department of Ophthalmology at Mount Sinai’s Icahn School of Medicine and retina services director at New York Eye and Ear Infirmary (NYEE). “These injections cause eye pressure to temporarily go up three times normal levels and while patients typically recover within minutes, we wanted to know the immediate impact on blood flow to the eye.”
Prof Rosen and his team analysed 40 eyes of 39 patients, all over 18-years-old with vision exceeding 20/100, could fixate, had no media opacities and were treated with bevacizumab (Avastin) or aflibercept (Eylea) for diabetic retinopathy, retinal vein occlusions, macular degeneration, retinal neovascularisation or radiation retinopathy. Perfusion density, thickness density and intraocular pressures (IOPs) were measured before and after injections were administered.
The findings, published in Retina, showed different areas of the eye were affected differently by the IOP spikes. Lead author, NYEE Clinical Associate Professor Alexander Barash reported finding significant (p < 0.05) decreases in angiographic perfusion density in most areas of the superficial and deep layers on macular OCTA, except for the fovea.
“The decreased angiographic perfusion density that is associated with increased IOP likely contributes to the acute decrease in visual acuity experienced immediately after injections,” he said, hypothesising that increased OCT thickness nasally may result from redistribution of fluid or fluid shifts that occur when the IOP changes.
This study could pave the way for doctors to pre-treat patients with medications to reduce their spikes in eye pressure after getting injections to protect them from possible long-term damage, said A/Prof Barash. “The findings may also lead doctors to more carefully consider the risks in patients with advanced glaucoma (who already have high levels of eye pressure) before treating them with injections.”