Battling for better eye care in NZ
Hamilton-based ophthalmologist and Auckland University senior lecturer Dr James McKelvie is leading the charge, together with several of his ophthalmology colleagues, to combat the postcode disparity for cataract surgery and obtain better eye care for all in New Zealand.
Following the publication of an open access article in the New Zealand Medical Journal reviewing access to cataract surgery and surgical intervention rates (SIR) in New Zealand, the Royal Australian and New Zealand College of Ophthalmologists (RANZCO) has backed Kiwi ophthalmologists’ calls for a nationwide threshold for cataract surgery, leading to general media coverage.
“Eligibility for public-funded cataract surgery in New Zealand is assessed on a weighted combination of visual acuity, cataract morphology and patient-reported quality of life,” wrote study authors Drs McKelvie, Corina Chilibeck, Jeremy Mathan and Stephen Ng. These are then combined to produce a clinical prioritisation and assessment criteria (CPAC) score ranging from 0 to 100. The CPAC threshold for cataract surgery is set by each district health board (DHB) and varies from a respectable 45 in Auckland to a poor 61 in the Southern DHB region and 60 in Waikato, Whanganui and the Bay of Plenty, according to data collected by the NZ Herald in the wake of the NZ Medical Journal article.
 Dr James McKelvie
Dr James McKelvie
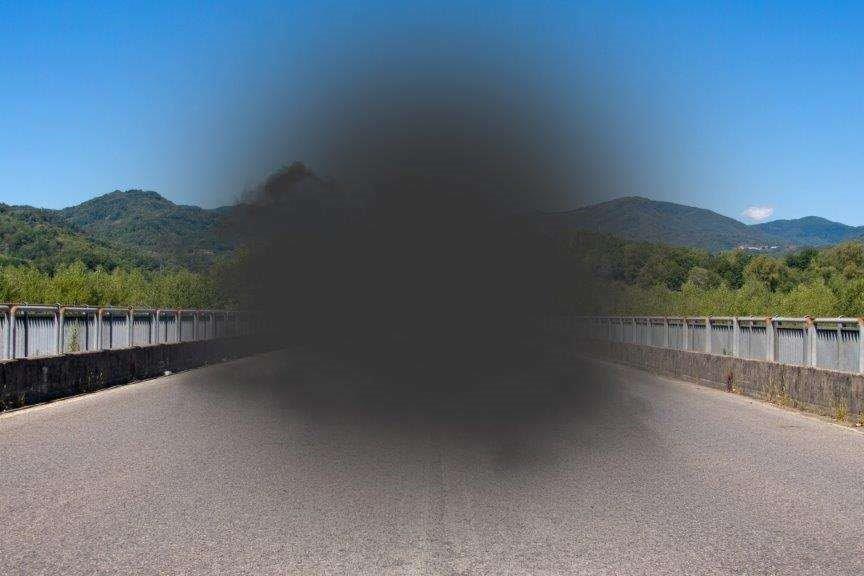
As well as highlighting the extent of the disparities that exist in the country, the research also identified that although the age and gender of patients prioritised for cataract surgery in New Zealand was similar to other OECD countries, our visual acuity thresholds were significantly worse. “The nationwide mean BSCVA of 6/30 (prioritised eye) at the time of prioritisation indicates that a significant level of visual impairment is required to access public-funded surgery in New Zealand,” with Māori and Pasifika having even worse levels, wrote Dr McKelvie et al. “Over one quarter of patients who were declined for surgery did not meet the visual acuity requirement for driving a private vehicle in New Zealand… (while) a small but significant number of patients who were declined for public-funded surgery had such advanced visual impairment they would be eligible for registration with Blind Low Vision New Zealand.”
The research also found significant differences in cataract surgery intervention rates across the country, with Auckland again topping the charts with over 700 surgeries per 100,000 population per year - more than double the national mean, which again was well below that of most other OECD countries.
The NZ Medical Journal cataract paper is one of a series of studies Dr McKelvie and his colleagues are working on to try to assess and thus better address eye care issues in New Zealand. “We’ve been working on this for some time; more than a couple of years,” said Dr McKelvie. “This paper looked at overall access to cataract surgery, but we have several other papers in the pipeline that characterise the increasing demand for ophthalmology and ophthalmic surgery in New Zealand.”
Solving the CPAC score disparities isn’t just about money either as the SIR rates show, he said. “Capacity is limited by a number of things, such as physical resources, but also efficiency and how we use those resources. Some operating theatres are doing more than 10 routine cataract surgeries in a half-day session whereas others will be doing as few as three. Some units have far more efficient systems than others. So, it’s also about developing tools to improve efficiency, while still maintaining a patient-centred service, low complication rates and excellent visual outcomes for patients.”
But introducing a single national CPAC threshold for cataract surgery is just one of a large number of changes that need to happen if New Zealand is to continue to meet growing demand for comprehensive public eye care across the country, he said. “There’s absolutely no question that we need to change the way that we do things, and that will involve innovative technology, new ways of working, involving nurses in different roles similar to the successful implementation of nurse anti-VEGF injectors by several DHBs and enabling better co-management of selected patients with optometrists, both in the hospital and in the community, so we manage patients in a more efficient and effective way.”
Until relatively recently, many ophthalmologists routinely saw cataract patients the day after their surgery. For routine cases, and in line with guidelines from the UK and elsewhere, this day-one review is now much less common, said Dr McKelvie. “As a result, we can safely reallocate thousands of clinic slots every year for other urgent, high priority and sight-threatening conditions. So, that’s a good example of how we can make better use of the finite resources we have. But changes like this require careful consideration and failsafe mechanisms to make sure we don’t compromise outcomes or add undue risks for the patient.”
Since publishing the cataract paper and being quoted widely in the media, Dr McKelvie said he’s had a lot of supportive comments from colleagues and patients across the country, so he’s hopeful the eye care community can work together to deliver positive change to benefit patients. “I have absolutely no doubt in my mind that we can deliver so much more even using the limited resources we have now; it’s just about new tools, innovation, and new ways of doing things.”
The full paper can be found at: https://www.nzma.org.nz/journal-articles/cataract-surgery-in-new-zealand-access-to-surgery-surgical-intervention-rates-and-visual-acuity