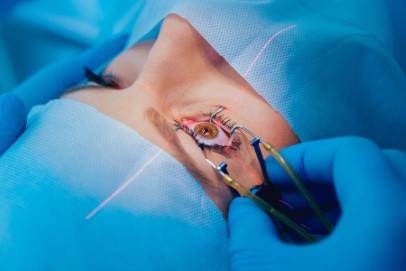
Cataract: reducing surgical complications risks
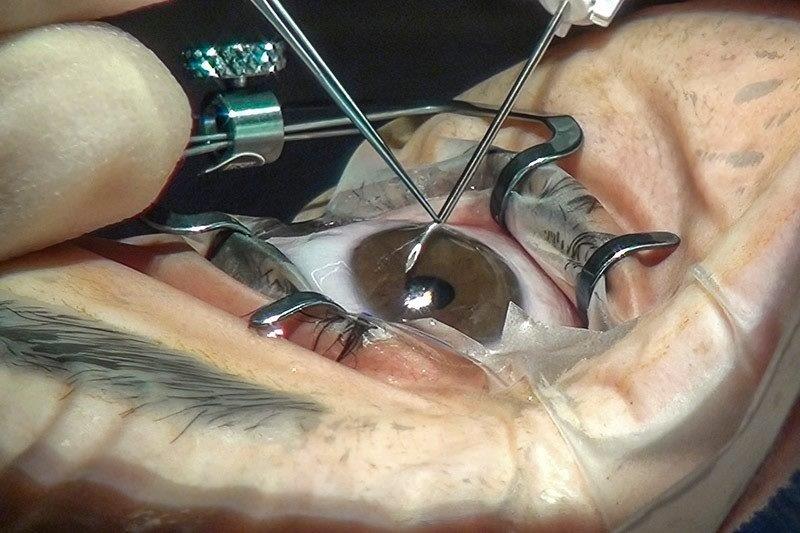
Despite major advances in phacoemulsification cataract surgery over the last 25 years, complications still occur, albeit at a relatively low rate. The Auckland Cataract Studies (ACS 2000-2020), led by McGhee et al, commenced with the appointment of the first anterior segment clinical research fellow, Dr Andrew Riley, to the University of Auckland in 2000. This initial prospective study of 500 procedures within the Auckland District Health Board (ADHB), demonstrated that significant intraoperative complication in phacoemulsification cataract surgery, such as posterior capsular tear, was 4.9% (registrars 5.4%, consultants 4.7%)¹. When compared to international studies in Australia, the UK and North America, this complication rate was similar to most teaching facilities.
The New Zealand cataract risk stratification system
Over subsequent years studies have sought to decrease the complication rate and also improve the management of cataract complications. By 2015 phacoemulsification technology had advanced significantly and complication rates had consequently reduced. At that time a further collaborative project was developed between Auckland University and the ADHB; a prospective study created to stratify risks of cataract complications in public teaching hospital settings. This was the beginning of the New Zealand Cataract Risk Stratification (NZCRS) system: a risk stratification system to reduce surgical complications of phacoemulsification cataract surgery.
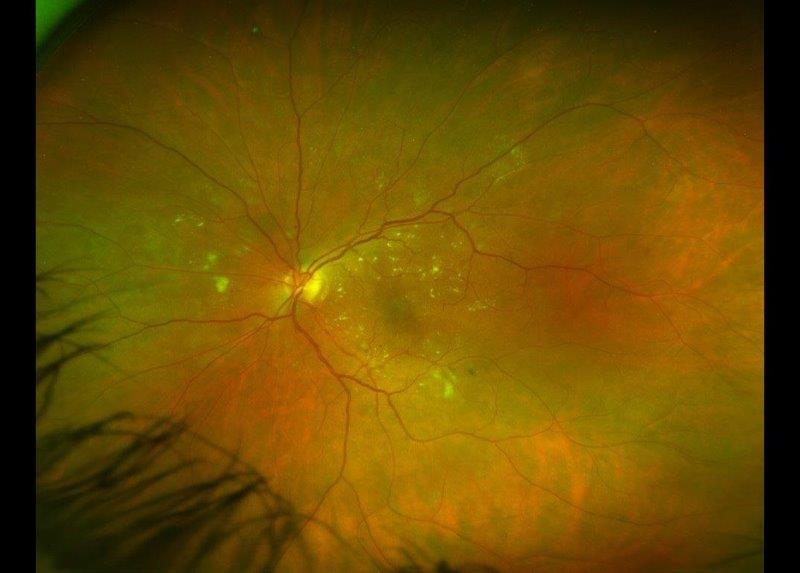
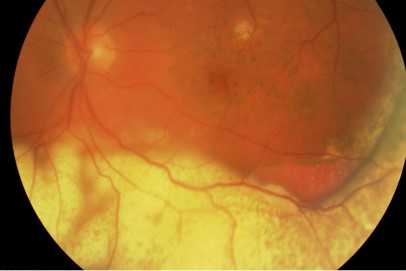
It has been long known that more advanced cataracts (eg. with dense or white nuclei) pose a greater risk of intraoperative complications. These more advanced cases are more typically encountered in public hospital services due to delayed presentation. Therefore, in analysing and comparing cataract surgery outcomes in public hospitals one always needs to consider (score) the case mix, especially as by comparison, single surgeon series in private practice often involve experienced surgeons operating on relatively less advanced or complex cataracts.
In 2015, Dr Bia Kim commenced a study assessing whether UK-originated stratification systems could be applied in New Zealand to reduce complications. A provisional observational study confirmed this was likely². A subsequent study, in which more complex cataracts were directed to more senior surgeons and less complex cataracts to trainee surgeons, validated that intraoperative complications could be reduced by as much as 40% using the Muhtaseb (UK) system³.
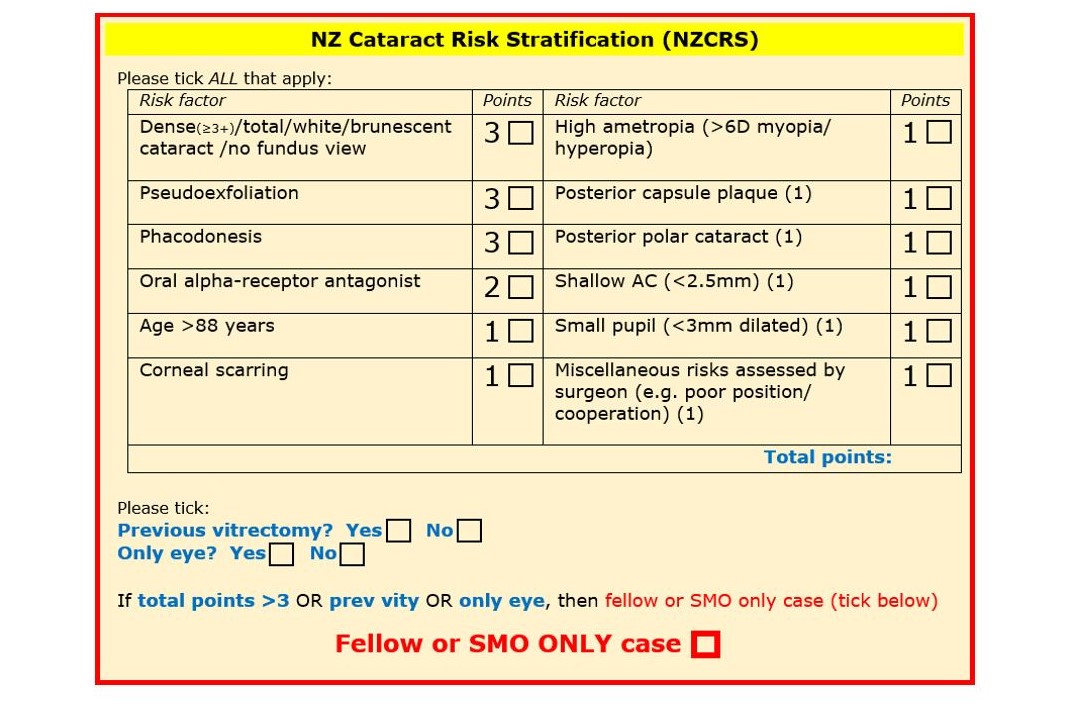
To further refine risk stratification systems for New Zealand, we built upon these early studies in 2017 to create the New Zealand Cataract Risk Stratification (NZCRS) system⁴. This system considers a number of key elements preoperatively that are known to increase the risk of complications (Fig 1). Factors such as cataract density, patient age, pseudoexfoliation and the use of alpha-receptor antagonists are considered. In the simplest terms, any patient with a risk score of >3 is allocated to a senior ophthalmic surgeon (consultant or fellow), whereas those with a score ≤3 can be operated on by any appropriately skilled surgeon, including trainees. Uniocular and vitrectomised eyes are allocated to a senior surgeon regardless of the risk score.
Results and conclusions
The Auckland Cataract Studies¹-⁵ have prospectively assessed 2500 patients, confirming surgical complications can be reduced dramatically with implementation of a risk stratification system and appropriate supervision in teaching hospitals. Indeed, in the latest cohort studied, following the implementation of the NZCRS system, overall intraoperative complications reduced by 64% compared with the baseline 2015 study (8.4% to 3.0%), and potentially sight threatening complications, such as posterior capsular tear and vitreous loss, reduced to less than 1%, ie. around 69% reduction from the 2015 baseline study and an 84% reduction from initial Riley et al studies of 2000-2001 (Fig 2.).
Fig 2. Intraoperative complications of phacoemulsification cataract surgery 2015-2018 (N=2000)
This increase in the safety of cataract surgery, both for surgeons in training and for patients, by using a simple three-minute pre-operative questionnaire, has proven so useful that the NZCRS system has now been adopted as the standard of care across the ADHB and has also been adopted in other parts of the Pacific. It is anticipated, this NZCRS system will continue to evolve and will become more widely used across New Zealand.
Ultimately, in a patient-centred-care environment, all patients have the right to know about the risks and benefits of surgery. They also have the right to know who will be carrying out or participating in the surgery and, specifically, to know whether the surgeon is still in training. The NZCRS study results provide excellent material for consent discussion and comfort for patients by them knowing that with appropriate stratification, the difference in surgical risks between an experienced and training surgeon (under direct supervision) is minimal. It has been policy for a number of years that all junior surgeons clearly inform patients they are still in their training phase and obtain personal consent for involvement in any surgical procedure. It is notable, therefore, that under the NZCRS system, in a fully informed setting the number of patients agreeing to undergo surgery with the participation of trainee surgeon has remained high and has not impacted on surgical numbers for trainee surgeons.
Cataract surgery per se remains the most common surgical procedure in New Zealand and indeed the world. Although phacoemulsification has very high levels of safety, cataract risk stratification systems such as NZCRS can reduce the risk of complications by >60%. Therefore, this can be considered an extremely safe procedure with severe, possibly sight-threatening complications, such as posterior capsular rupture or vitreous loss, now being less than 1%.
References
- Riley AF, Malik TY, Grupcheva CN, Fisk MJ, Craig JP, McGhee CN. The Auckland cataract study: co-morbidity, surgical techniques, and clinical outcomes in a public hospital service. Br J Ophthalmol. 2002 Feb;86(2):185-90
- Kim BZ, Patel DV, Sherwin T, McGhee CN. The Auckland Cataract Study: Assessing Preoperative Risk Stratification Systems for Phacoemulsification Surgery in a Teaching Hospital. Am J Ophthalmol. 2016 Nov;171:145-50
- Kim BZ, Patel DV, McKelvie J, Sherwin T, McGhee CNJ. The Auckland Cataract Study II: Reducing Complications by Preoperative Risk Stratification and Case Allocation in a Teaching Hospital. Am J Ophthalmol. 2017 Sep;181:20-5
- Han JV, McGhee CN. When is a complication a complication in contemporary cataract surgery? Clin Experiment Ophthalmol. 2018 Jan;46(1):7-10
- Han JV, Patel DV, Wallace HB, Kim BZ, Sherwin T, McGhee CNJ. Auckland Cataract Study III: Refining Preoperative Assessment With Cataract Risk Stratification to Reduce Intraoperative Complications. Am J Ophthalmol. 2019 Jan;197:114-20
Dr Jina Han is a clinical research fellow in cornea and anterior segment diseases in the Department of Ophthalmology, Auckland University. Professor Charles McGhee is chair of ophthalmology at Auckland University, director of the National Eye Centre and immediate past-president of the Asia Pacific Academy of Ophthalmology.