Rhodes scholar researching RNA-editing
Dr Lewis Fry followed in the footsteps of Lorde, Lydia Ko and Eliza McCartney in winning the prestigious AIMES (Arts, Innovation, Music, Education, Sport) Supreme Award that rewards excellence in young people on Auckland’s North Shore.
The AIMES Emerging Talent Award he received in 2014 enabled him to undertake a year-long project into vision loss from glaucoma, whilst studying medicine in Melbourne. He went on to successfully apply for a Rhodes Scholarship at Oxford University and, in 2017, he won the AIMES Education Award, as well as the overall title and $30,000 prize.
In late 2019, Dr Fry used AIMES funding to attend the Cold Spring Harbour Laboratory meeting in New York where he presented his genome editing research. He left his lab to answer some questions for NZ Optics from a chilly Oxford.
What is your earliest eye-related memory?
As I went through school, I progressively struggled to see the whiteboard. I had a pair of glasses, but as a teenager with braces, wearing these was a step too far for me! When I finally committed to wearing them after a few years, I finally discovered I could read the rugby score on TV and my batting in cricket vastly improved as I could see the ball. It was a very small but valuable insight into how even small improvements to vision can make a significant difference.
What drew you to ophthalmology?
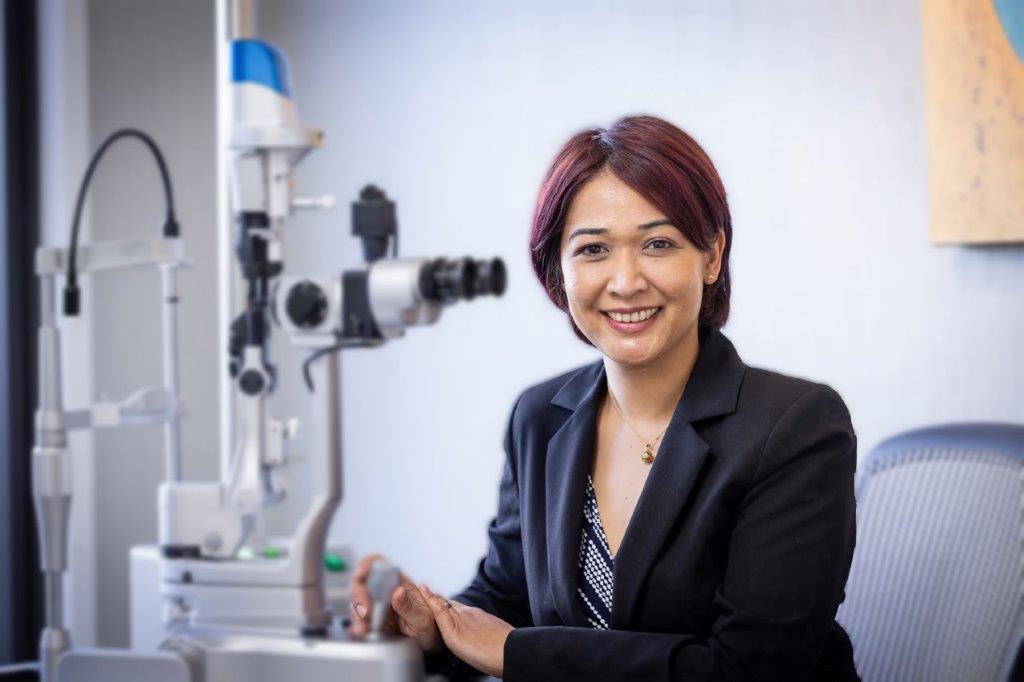
The first thing that captured me was the beauty of the eye – I saw an iris in the slit lamp and thought it was the most intricate thing I’d seen in the human body. I felt the same when I then saw Ramon y Cajal’s early drawings of the histology of the retina. I spent a week with Prof Helen Danesh Myer and her colleagues in Auckland in my holidays, and also six weeks working in a rural clinic in Eswatini. In vastly different settings, I saw satisfied patients post-operatively and warm long-term doctor patient relationships. The combination of medicine, surgery and neuroscience seemed like a perfect fit for me.
What was your educational path to where you are today?
I left school in Auckland to study medicine at Monash University in Melbourne as they offered a full scholarship for my degree. During that time, I spent an influential year in a lab in the Centre for Eye Research Australia doing a Bachelor of Medical Science, working on glaucoma pathophysiology. I really enjoyed the challenges of research and realised I wanted to do a PhD. After graduating and working in Melbourne as a junior doctor, I applied successfully for a Rhodes Scholarship to the University of Oxford to pursue that dream.
Where are you based now?
I’m now based at the University of Oxford. I work in the John Radcliffe Hospital in the Nuffield Department of Clinical Neuroscience in Professor Robert MacLaren’s ophthalmology lab. Prof MacLaren is currently leading clinical trials for gene therapy in choroideremia, X-linked retinitis pigmentosa and macular degeneration, while in the lab we develop gene and cell-based treatments for inherited retinal disease.
Whose mentorship have you particularly valued?
I’ve been privileged to have many mentors, all of whom have generously given me time and new perspective. Prof Helen Danesh-Myer persuaded me to consider ophthalmology and has always warmly encouraged me on my path so far. I was lucky to be supervised by Professor Jonathan Crowston and Associate Professor Peter van Wijngaarden in Melbourne - a superb duo who first showed me the workings of what it means to be a clinician-scientist and how to ask interesting questions in medicine. I continue this now with the guidance of Prof Robert MacLaren. And there are too many others to mention!
How was the Cold Spring Harbour Laboratory Meeting in New York?
This was a fantastic meeting, and I have developed a couple of interesting collaborations with scientists from the USA directly from this. I’ve also been engaging with the governance of genome editing. This has become a controversial issue since scientists in China secretly edited human embryos in an unregulated manner. I attended a meeting of the National Academy of Sciences in London where policy is being developed to produce a global consensus on genome editing regulation and ethics.
Could you summarise your current main area of research?
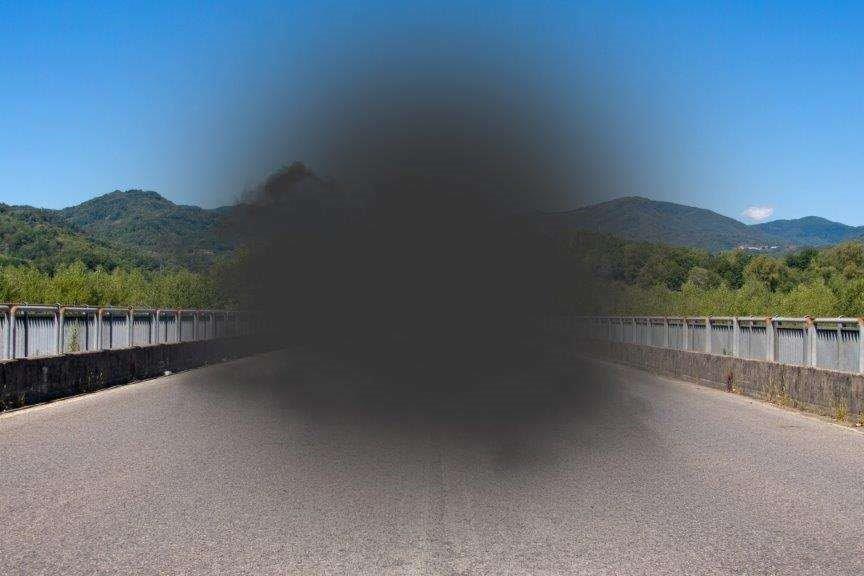
Mutations in genes cause the death of cells in the retina in inherited retinal diseases such as retinitis pigmentosa, a common cause of irreversible blindness in people of working age. We are researching whether editing these genes to correct the mutations might work to treat some of these diseases. For this we are using CRISPR-Cas, a technology that allows for genes to be specifically targeted and edited. RNA is the messenger molecule that helps translate the DNA of genes to become protein. I have been developing an approach where we could edit the RNA of a gene involved in Usher syndrome, which causes both blindness and deafness. We hope that correcting this mutation would prevent the death of cells in the retina and therefore prevent blindness for patients with Usher syndrome.
What are your goals for 2020 and beyond?
The coming year is a crunch year for my research – I have a few big experiments and collaborations planned that I need to work well and that will be important for my research career. I hope I can finish my thesis soon after 2020. Beyond that, it will be back to balancing research and medicine, and I hope to shortly start training in ophthalmology. Long term, I hope this training in genetics will set me up well for a career bridging ophthalmology, genetics and research in New Zealand.