Squint Club 2019: report
The Australian and New Zealand Strabismus Society (ANZSS), better known as the Squint Club, held their 2019 meeting at the Melbourne Children’s Hospital.
Local orthoptist Alex, kindly showed us around this great new facility, featuring a spectacular atrium and “creature” sculpture. The ophthalmic outpatient department was equipped with state-of-the-art clinics and a very child-friendly waiting room with outdoor play access, low seating and even a meerkat enclosure - a brilliant way to keep the little ones amused prior to assessments.
The ANZSS meeting also didn’t disappoint, providing a lively discussion forum with a good mix of lectures, live cases and practical pearls from the interactive Q&A sessions with the audience.
Difficult cases
The first case involved a large, variable abnormal head posture (AHP) with latent nystagmus and a variable, horizontal XT. Invited speaker Dr Jonathan Homes from the Mayo Clinic in the US, explained how the variable measurements in gaze positions drove head posture and suggested asymmetrical recession/resection. Dr Lionel Kowal reminded us to test uniocularly, as in fixation maldevelopment nystagmus (FMDN) the AHP will change dependent upon the fixing eye. He also suggested we correct strabismic deviation with large prisms in clinic to see if the AHP improves.
Nystagmus featured again in a periodic alternating nystagmus case presented by Drs Shivanand Sheth, Cheefoong Chong and Even Heinecke. Dr Kowal and Associate Professor Larry Abel explained how a face turn may only alternate in 50% of cases and is often independent of the fixing eye, whereas in infantile esotropia, fixation drives head turn.
Another complex case with an acquired multi-directional oculo-palatial nystagmus and oscillopsia had been given Botox to the horizontal recti, which improved the amplitude of the horizontal component of the nystagmus. Dr Holmes suggested rather than consider surgery, try Botox on the vertical recti to see if this helps the vertical component, while still leaving torsional movement.
This case and another live case, featuring a child with a traumatic IVn palsy, provided a good reminder that in any neurological case we need to wait the full six months before checking for neurological recovery prior to considering anything invasive.
Another interesting case from Drs Sheth, Sheetal Shirke, Phoebe Moore and Kowal featuring neurogenic Brown’s and superior oblique palsy reminded us that neurological Brown’s often doesn’t improve whereas mechanical often does. Dr Sheth also commented that you can do a finger forced duction test (FDT) through the lower lid to push the globe in adduction and abduction to compare and quickly check in clinic. Later in the meeting, a useful suggestion for treating a painful Brown’s patient was trying a cocktail of local anesthesia plus a steroid injection to the trochlea to help with pain.
Retinal misrepresentation
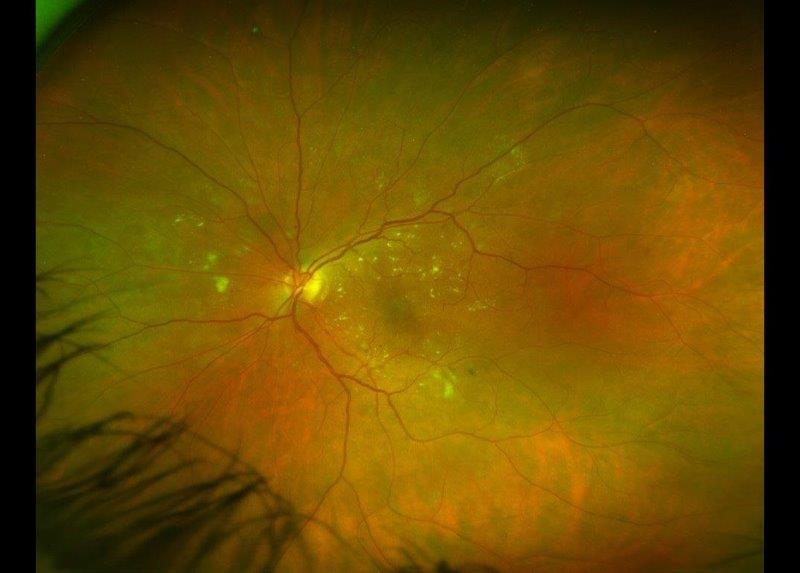
Orthoptist Associate Professor Kyle Arnoldi from New York and Dr Holmes also discussed macula diplopia from epiretinal membrane (ERM) and retinal surgery causing retinal misrepresentation, a condition we are seeing more frequently now.
From an audit of her patients, A/Prof Arnoldi said 9% had diplopia at diagnosis of ERM, while 2% also had metamorphopsia. She gave three diopters as the magic number to look for as the majority manifest as small comitant vertical deviations (mean 2.6) with a discrepancy between the subjective and objective angle. A good trick to watch for is the image appears to move on uniocular viewing and check with the ‘light on/lights off’ test.
One thing I’ve also come across in my practice is patients who can have vertical diplopia without any manifest vertical strabismus. Prisms don’t help these patients as they ‘eat up’ prisms at each visit so fogging or monovision is often the best option.
Research updates
Dr Holmes presented some of the latest research from the Paediatric Eye Disease Investigator Group (PEDIG), including an exotropia treatment study into over-minus glasses, the new hyperopia treatment study (HST1) and early vs late prescription of glasses and the risk of consecutive esotropia and a parallel study for older children aged 3-5 years. Though the latter had to be cut short due to low enrollment numbers, researchers found a failure to treat showed no statistical difference between those observed and those treated. Even the treated group showed a low rate for accommodative ET, so it’s okay to just observe, but if we do, we need to remind parents to refer if they see any crossed eyes or change. Pleasingly, those not prescribed glasses continued to improve compared to those given glasses (42% vs 17% to reduce by 1 dioptre). The team used a blue temperature gauge ‘smarties’ stick-on button on the glasses temple to monitor compliance; a clever idea which will help with future compliance studies.
Another practical study which had all the orthoptists talking was presented by Juliette Duck and Associate Professor James Elder regarding exercise-induced esotropia cases. To elicit the phenomenon, you have to fully tire the young patients out - they ran up and down 25 flights of stairs! – and check CT scans as they could have a form of idiopathic Arnold-Chiari malformations. Duck postulated exercise-induced esotropia could be due to a compression phenomenon, impaired-venous outflow or CSF inflow issues, and won the prize for the best non-ophthalmologist talk!
More practical pearls
A/Prof Arnoldi also generated a lot of good discussion with a series of cases on partial third cranial nerve palsy where the inferior rectus (IR) proved the hero. Careful examination of ocular movements and noting any incommitance of height of the IR action led to a different diagnosis and further investigation.
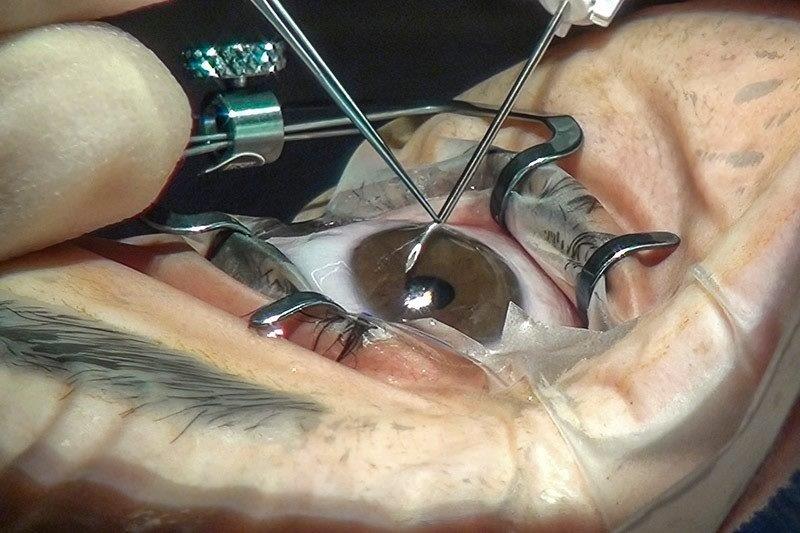
Orthoptists can also improve surgical outcomes through good pre- and post-operative testing, she said. Determine the fusion potential to assess control and support and ameliorate patient expectations and confirm the type of retinal correspondence (NRC) testing to check for ARC.
Dr Holmes explained how with the newer transposition for strabismus technique, you theoretically should get hypo and incyclotorsion when you transpose the superior rectus but in reality, you don’t. Referring to another PEDIG study in intermittent exotropia control in under three-year-olds and three to 10-year-olds for patching versus observation, researchers found the rate of deterioration low, just 15%. Many parents report deterioration, but it’s not true clinical deterioration, so don’t rush to surgery, he said, as some kids lose stereoacuity at one visit but regain it at the end.
There are various studies relating to patching vs over-minus glasses vs surgery. At present, patching is still a reasonable strategy in the three to 10-year-old group, but there’s insufficient evidence in the younger group. With regard to over-minus, PEDIG ran a pilot study using -2.50DS and found it seemed to help acutely compared with controls at eight weeks so is undertaking a larger, longer-term study.
Rather than the Newcastle Control Score, Dr Holmes uses the Office-based Control Score for assessing control in intermittent exotropia. The patient-centred questionnaire PEDIG has produced and tested was really interesting as I’ve been wanting to introduce something similar in my clinic. I will definitely be accessing their short forms, which are freely available on the PEGIG website.
All those I spoke to, said this is one of their favourite meetings to attend. With the calibre of talks, the practical nature of the varied presentations and the lively, open discussion format, I must say, I agree.
Sally-Anne Herring is a UK-trained orthoptist with more than 30 years’ experience in orthoptics, paediatrics and neurophthalmolgy, now working in New Zealand’s Hawke’s Bay and providing additional locum cover further afield. She is an active member of BIOS, NZOSI and OA, served as secretary of the NZOSI from 2006 to 2017 and is currently NZOSI’s AHANZ representative.