Vitreo-retinal developments
Pneumatic retinopexy versus vitrectomy for the management of primary rhegmatogenous retinal detachment outcomes randomised trial (PIVOT)
Hillier RJ, Felfeli T, Berger AR, Wong DT, Altomare F et al.
Ophthalmology. 2019 Nov;126(11):e84
Design
Randomised controlled trial of 176 patients with rhegmatogenous retinal detachments. Patients had a retinal break or breaks in detached retina within one clock hour above the eight and four o’clock meridians and were randomised to undergo either pneumatic retinopexy (PnR) or pars plana vitrectomy (PPV).
Outcome
Primary anatomic success was higher in the PPV arm compared to PnR arm (93.2% vs. 80.8%). However, visual acuity improvement was superior in patients who underwent PnR compared to PPV at 12 months (79.9 vs. 75.0 letters). Patients in the PnR arm also had less vertical metamorphopsia. More patients in the PPV group had cataract surgery.
Limitations
15% of patients did not complete the one-year vision assessment. There was also a disparity in the number of retinal breaks at baseline, with more breaks in the PnR arm, which may have biased anatomical success in favour of the PPV arm.
Comment
This is a well-designed comparison of two different procedures to repair suitable retinal detachments. Patients who had PnR had slightly better vision and less distortion compared to patients who had PPV, albeit with a lower primary success rate. It’s important to recognise that there is an art to PnR, and that this centre in Toronto has more or less perfected it. Although PnR patients managed to avoid the operating theatre if their initial procedure was successful, I would argue that it is a more uncomfortable procedure compared to PPV.
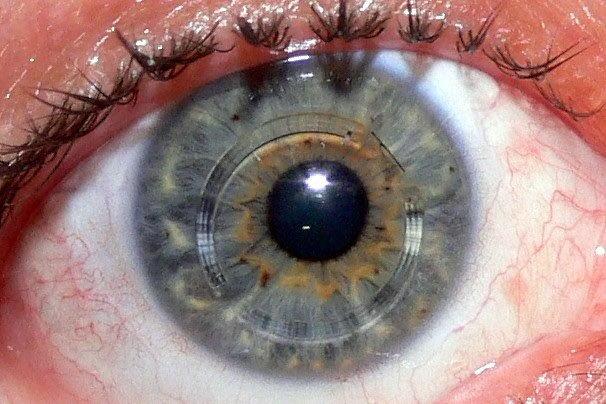
Comparison between ultra-widefield pseudocolor imaging and indirect ophthalmoscopy in the detection of peripheral retinal lesions
Fogliato G, Borrelli E, Iuliano L, Ramoni A, Querques L, Rabiolo A, Bandello F, Querques G
Ophthalmic Surg Lasers Imaging Retina. 2019 Sep 1;50(9):544-549
Design
Prospective, observational, cross-sectional study of 37 eyes with peripheral retinal lesions predisposing to rhegmatogenous retinal detachment. Ultra-widefield (UWF) imaging and dilated fundus examinations were performed and inter-modality agreements compared.
Outcome
The level of agreement was excellent in both the ophthalmoscopy-based and UWF-based assessment. The UWF-based evaluation had a sensitivity of 89.2% in detecting peripheral retinal lesions overall, which was lowest in the inferior sector.
Limitations
The main limitation of this study was the small number of enrolled eyes. The UWF images were also taken by an ophthalmologist who, more than likely, invested considerable time and effort to obtain the best images possible.
Comment
The use of UWF imaging is gaining in popularity in both the community and hospital setting and this study validates its utility in detecting peripheral retinal lesions predisposing to rhegmatogenous retinal detachments. In this study, the UWF images were taken with the Optos California device, and amazingly, prior to pupillary dilation. As with most imaging modalities, obtaining good UWF images requires good patient cooperation and image quality may be affected by artefacts from the eyelids and lashes. One of the main limitations of preceding UWF devices was distortion of the peripheral retina, giving an artificially stretched look. This distortion is intrinsic to UWF devices and is due to the ellipsoidal mirror used to obtain a broad viewing angle. However, recent advances in software algorithms have overcome this limitation and should improve image quality.
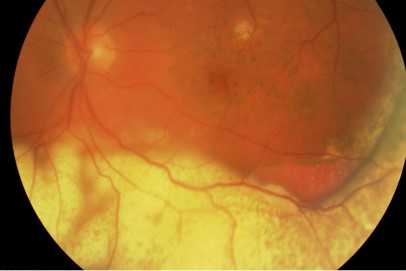
Pneumatic displacement of submacular haemorrhage with subretinal air and tissue plasminogen activator: initial United States experience
Sharma S, Kumar JB, Kim JE, Thordsen J, Dayani P, Ober M, Mahmoud TH
Ophthalmol Retina. 2018 Mar;2(3):180-186
Design
Retrospective, interventional case series of 24 eyes affected by submacular haemorrhage (SMH) secondary to age-related macular degeneration or polypoidal choroidal vasculopathy. Patients underwent displacement of SMH with pars plana vitrectomy, subretinal injection of air and tPA (125 mcg/mL), partial fluid-air exchange with gas tamponade, and anti-vascular endothelial growth factor (VEGF) injection.
Outcome
At three months after surgery, complete displacement of SMH from the fovea was achieved in 24 eyes (100%), beyond the arcades in 75% and beyond the equator in
20%. Mean pre-operative and post-operative visual acuity was 20/1783 and 20/141 respectively.
Limitations
The lack of a control group prevents adequate comparison of the study outcomes with the natural history of SMH or other management options (such as anti-VEGF injections alone).
Comment
SMH is a devastating complication, which often portends a poor visual prognosis. Subretinal blood can quickly induce irreversible retinal damage through different mechanisms, including trauma to photoreceptors from clot retraction, direct iron toxicity and prevention of normal physiological function through a barrier effect. Hence, it makes sense to displace blood from the macula with haste. Numerous treatment strategies and a wide variation of displacement success has been reported. However, there is no consensus about the optimal management. This technique of injecting subretinal air at the time of tPA injection during PPV seems to be effective and can consistently displace SMH away from the fovea and even out to the periphery. Further studies with larger patient cohorts are awaited.
Dr Joel Yap is a consultant ophthalmologist and vitreo-retinal specialist at Auckland DHB and Counties Manukau DHB. He completed his vitreo-retinal fellowship last year at the University of Toronto in Canada is currently a visiting vitreo-retinal specialist for Eye Doctors at Ascot Hospital and Botany Junction.