Case study: There was an old lady who fly sprayed her eye…
A peculiar case of corneal oedema in an elderly patient, highlighting the importance of obtaining collateral history when there’s no obvious cause.
An 83-year-old female presented with a four-month history of right eye floaters and reduced vision. She denied any pain, recent ocular trauma, chemical injury or contact lens wear.
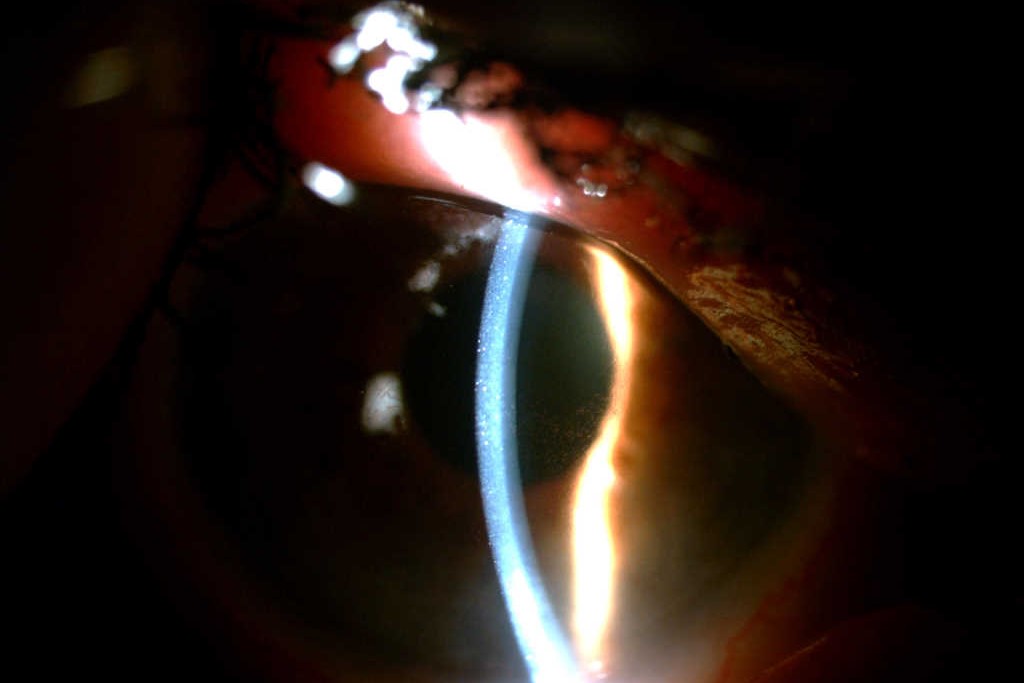
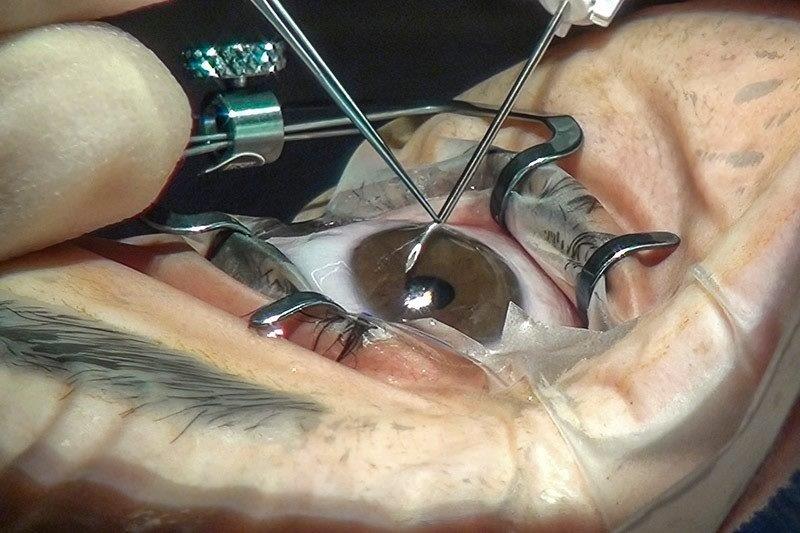
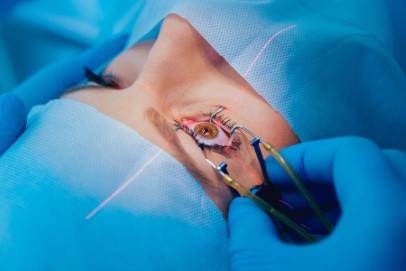
Her best corrected visual acuities (BCVA) were 6/24 in the right eye and 6/15 in the left. Intraocular pressures were 9mmHg right and 10mmHg left. The cornea was noted to be significantly decompensated with generalised epithelial microcysts and bullae, and Descemet’s folds, but without obvious guttata, epithelial defect, infiltrate or limbal ischaemia (Fig 1 and 2). The right anterior chamber was deep and quiet. There was a well-placed intraocular lens in the capsular bag from previous routine, uncomplicated right cataract surgery seven years prior. Dilated fundal examination was normal. The left eye was unremarkable apart from posterior vitreous detachment and moderate cataract. B-scan of the right eye demonstrated posterior vitreous detachment without other chorioretinal or vitreous abnormality. Ocular coherence tomography (OCT) of the cornea showed epithelial splitting with increased central thickness of 653µm in the right eye compared with a normal corneal OCT and central thickness of 550 µm in the left.
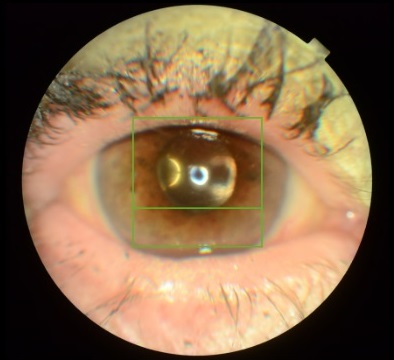
Fig 1. Photograph of the right eye with corneal oedema at presentation, with cross section of OCT scan
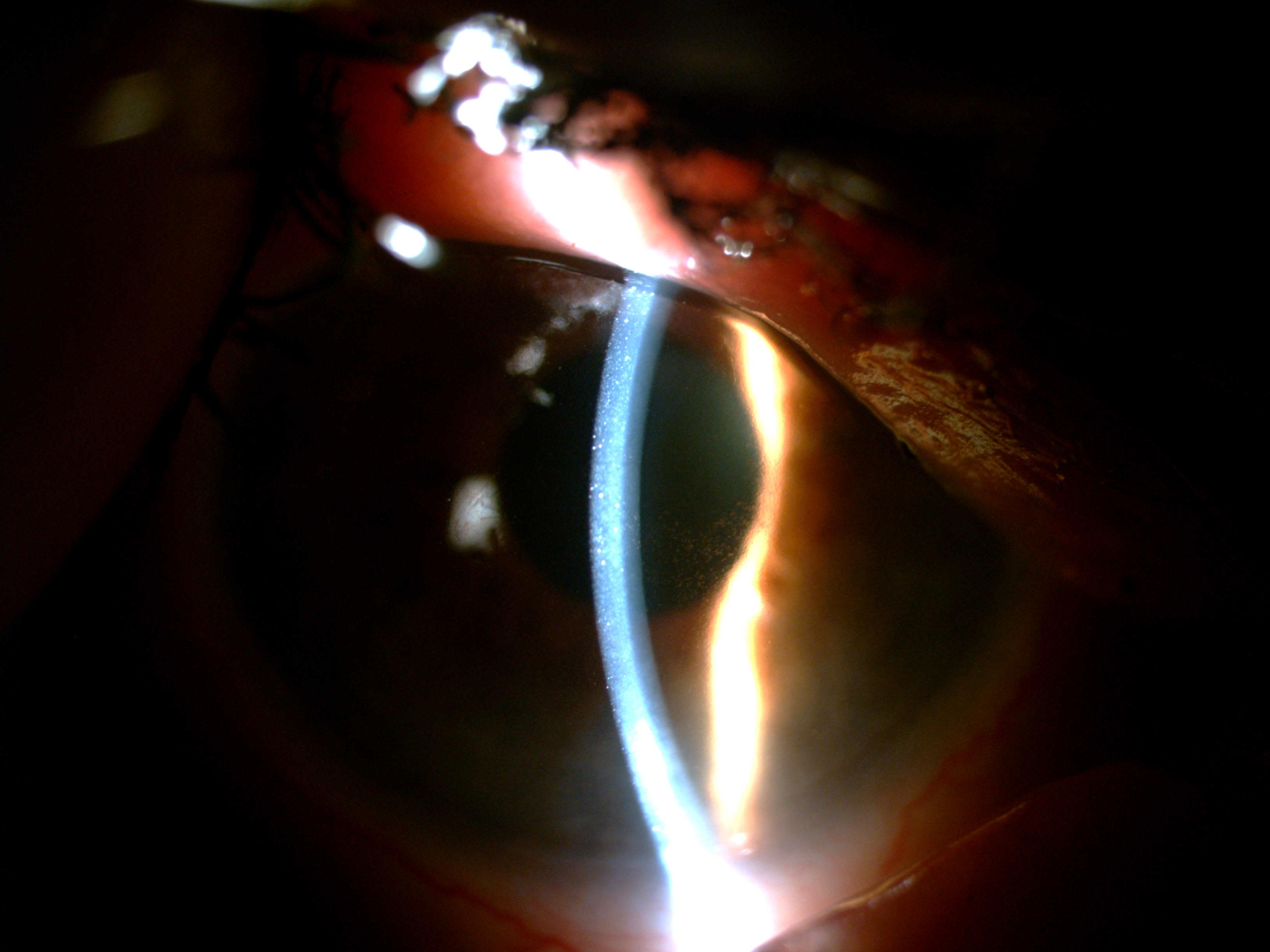
Fig 2. Angled slit beam demonstrating corneal epithelial microcysts in the right eye
Prednisolone acetate 1% drops were commenced four times daily.
At two weeks follow up, the patient reported persistent right eye floaters with unchanged BCVA and examination findings. We subsequently received a letter from her general practitioner (GP) reporting that the patient had cognitive impairment which was not noted in her history. The GP explained our patient had confided that she believed the floater in her left eye was a living being and her friend, and the new floaters in her right eye were a threat to her friend. As such, she has been using fly spray on her right eye in an attempt to get rid of the new floaters since their onset. Thus, it was deduced that the fly spray was then the likely offending agent in her right corneal decompensation.
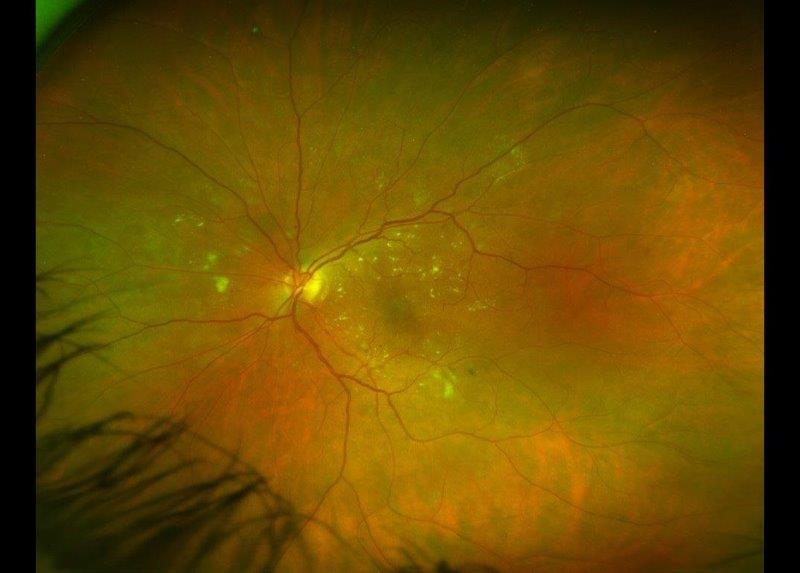
At follow-up we observed slow progressive resolution of the corneal decompensation (Fig 3). Fortunately, our patient had good vision in her left eye allowing for non-intervention in the right eye.
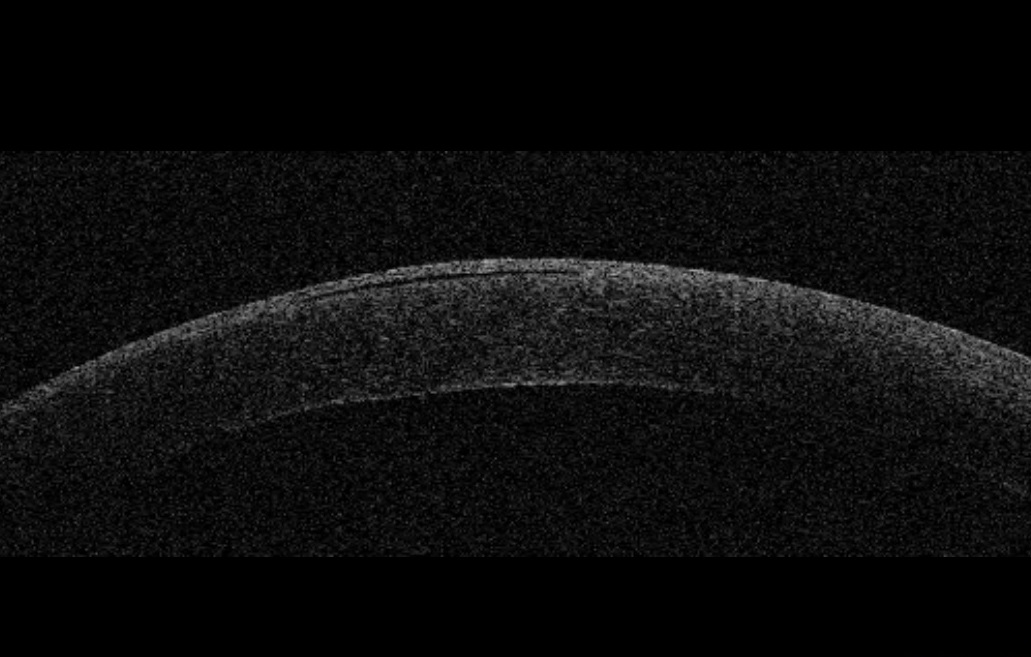
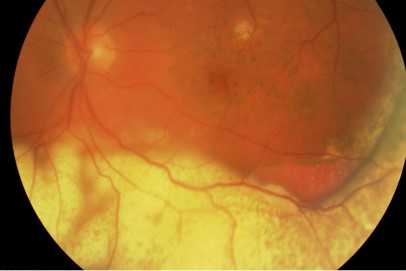
Fig 3. OCT cornea of the same eye below the visual axis showing a subepithelial bulla
Discussion
There is a broad range of causes of corneal oedema: corneal dystrophies, glaucoma, inflammation, infection, ocular surgery, chemical injury or trauma (Costagliola, 2013).
The main active ingredient commonly used in fly sprays is synthetic pyrethroids which paralyse the fly’s nervous system. Synergists such as piperonyl butoxide and N-octyl bicycloheptene dicarboximide delay metabolism of the active ingredients therefore prolonging their action (Castles, 2017). All of these chemicals are known to be irritants of the skin and eyes, although the exact effects of ocular exposure are unknown.
Identification of the cause of corneal oedema may be difficult in patients with cognitive impairment. Further information could be obtained from GPs and/or a close relative or friends (Dyer, 2018). Enquiries should be made to ascertain any possibility of chemical or mechanical injury that may have precipitated the corneal oedema. It is also possible to have the patient observed for any behaviour that may give rise to injury.
We thank the patient and her family for their consent to publish this case report.
References
- Castles B. Fly sprays 2017 [updated 27 October 2017]. Available from: https://www.consumer.org.nz/articles/fly-sprays
- Costagliola C, Romano V, Forbice E, Angi M, Pascotto A, Boccia T, et al. Corneal oedema and its medical treatment. Clin Exp Optom. 2013;96(6):529-35
- Dyer AH, Foley T, O'Shea B, Kennelly SP. Cognitive assessment of older adults in general practice: the collateral history. Ir J Med Sci. 2018;187(3):683-7
Dr Kelvin Ngan is a non-training ophthalmology registrar with Nelson Marlborough District Health Board serving Nelson and Wairau Hospitals, with prior ophthalmic experience in Wellington and Hawkes Bay.
Dr Sacha Moore is a consultant ophthalmologist with the Nelson Marlborough District Health Board. He specialises in cornea and anterior segment surgery.