AUSCRS 2019 in Middle-earth
This year was the 23rd Australasian Society of Cataract and Refractive Surgery (AUSCRS) meeting and it was the third time it was held in Queenstown. Well attended by New Zealand ophthalmologists, the theme for this year’s meeting was Crystal Clear and continued AUSCRS’ unique format with casual dress, unusual session themes and the opportunity to meet and talk with overseas invited speakers.
This year’s more unique sessions included the Logfire chat, where industry representatives and senior ophthalmologists discussed future trends and innovations in cataract and refractive surgery; Head to Head, which allowed cataract surgeons to argue the case for their preferred intraocular lens (IOL); and an interesting session on life-work balance in ophthalmology. Now part of AUSCRS traditions, speakers dressed up in a variety of costumes largely themed on Queenstown’s adventure reputation.
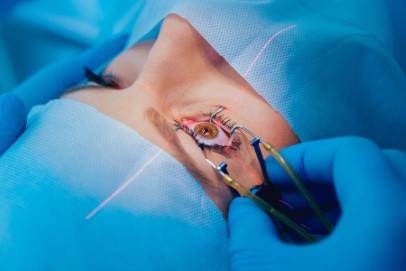
IOL exchange techniques
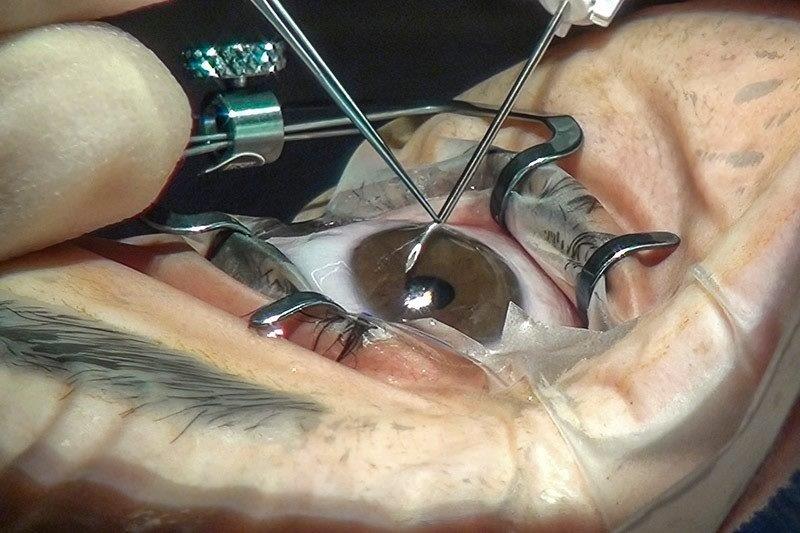
The welcome from AUSCRS’ president, Professor Graham Barrett was followed by an amazing lecture from Dr Steven Safran on IOL exchange techniques. Dr Safran is very active on social media and YouTube and has an extensive library of surgical videos. He covered many advanced techniques for late IOL exchange, including methods for extracting well-stuck IOL haptics from the equator of the lens capsule, the late rotation of toric IOLs and posterior vitrectomy for anterior segment surgeons. He also summarised techniques he’s used for IOL fixation in the absence of lens capsule support, solving negative dysphotopsias and dealing with decentred IOLs.
Complications, torics and presbyopia
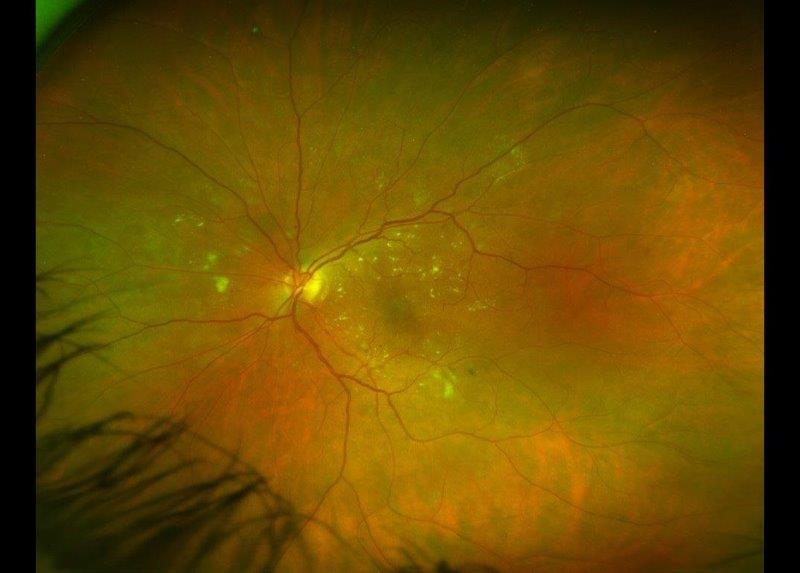
The session on anterior surgical complications included loss of the endothelial graft during DMEK, fixation of a HumanOptics artificial iris, how useful vitrectomy for opacities is in unhappy IOL patients, operating on a cataract caused by vitreous floater laser treatment and cataract surgery with zonule dehiscence.
This was followed by a session on toric IOLs including using low cylinder (T2) toric IOLs and comparing cylindrical power and axis calculation methods. So far, none of methods that include direct measurements of total corneal astigmatism appear to outperform the Barrett Toric Calculator. Prof Barrett also talked about using toric IOLs in post-laser refractive surgery patients using his new True-K Toric calculator, which includes posterior corneal astigmatism measurements with the IOLMaster 700.
The final session of the first day focused on presbyopia IOLs. Papers were presented that compared extended-depth-of-vision (EDoF) to other IOLs and examined EDoF IOLs that attach to the edges of the anterior capsulorhexis. The purpose of EDoF IOLs is to give patients some useful, unaided, near vision while causing minimal night driving and dysphotopsia issues. One presentation compared the Zeiss AT LARA EDoF IOL with a monofocal IOL and found only a mild increase in glare and halos with the AT LARA but significantly better intermediate and near unaided vision. A similar conclusion was reached in a study comparing the Oculentis Comfort EDoF IOL with a monofocal IOL.
Which IOLs, why FLACS, what balance?
The highlight of the second day was the Head to Head session about preferred presbyopia-correcting IOLs with the winner decided via table tennis games! We then debated the merits of femtosecond laser-assisted cataract surgery (FLACS) which, while interesting, confirmed there were no convincing, scientifically proven advantages justifying the extra cost.
Following a session on how to go about achieving some work-life balance, the day finished with a session on managing cataract and IOL surgery complications, lens surgery for angle closure glaucoma and MIGS. Dr Safran also presented on managing dislocated IOLs.
Tear film risks, corneal pearls and more
The last day focused on refractive surgery and included discussion about the use of tear film inflammatory markers, such as MMP9, and tear film osmolarity as possible risk factors for post-LASIK keratectasia. It was proposed a system be developed that could detect sub-clinical keratoconus using just tear film analysis. The use of epithelial thickness maps for detecting sub-clinical keratoconus in refractive surgery candidates was also discussed.
Another highlight was the corneal pearls session, which included recent research on ocular surface disease, keratoconus and cataract surgery. Also discussed was post-cataract residual refractive error treatments, when to use multifocal IOLs in post-laser refractive surgery patients and managing traumatic cataracts.
The wonderful gala dinner brought the conference to a close, with most delegates embracing the Lord of the Rings theme. The highlight: watching Gollum on the dance floor - a truly scary sight!
Dr David Kent is a consultant ophthalmologist with Fendalton Eye Clinic and Christchurch Eye Hospital. He is a member of both the American and Australasian Societies of Cataract and Refractive Surgery, and the New Zealand AUSCRS council representative.