Clinical pearls from GSLS 2019
Now in its eleventh year, the Global Speciality Lens Symposium (GSLS), held annually in Las Vegas, is a unique conference focused on enabling eye care practitioners to make the best use of modern speciality contact lenses to help a wide range of patients.
While the more than 1000 attendees and exhibitors were predominantly from the US, the conference truly lived up to its ‘global’ title with delegates from 35 countries represented, travelling from as far afield as Europe, Asia, Australia, New Zealand and South America.
I have been aware of this conference for some time, but 2019 presented my first opportunity to attend, so these are my impressions as a first-time attendee. As a British optometrist, now living in Canada and working at the Centre for Ocular Research & Education in Waterloo, Ontario, much of my personal work experience and research has been focused on matters relating to soft contact lenses, with a touch of rigid gas permeable fitting and dry eye management thrown in. Given that background, I had high expectations of learning a great deal from the three-and-a-half-day conference.
That view turned out to be correct. As the conference drew to a close, I was left with a head and note pad full of the most up-to-date information and valuable clinical pearls to take back into practice. The most prominent topics covered were scleral lens fitting, orthokeratology (ortho-k) and myopia control.
Scleral lenses
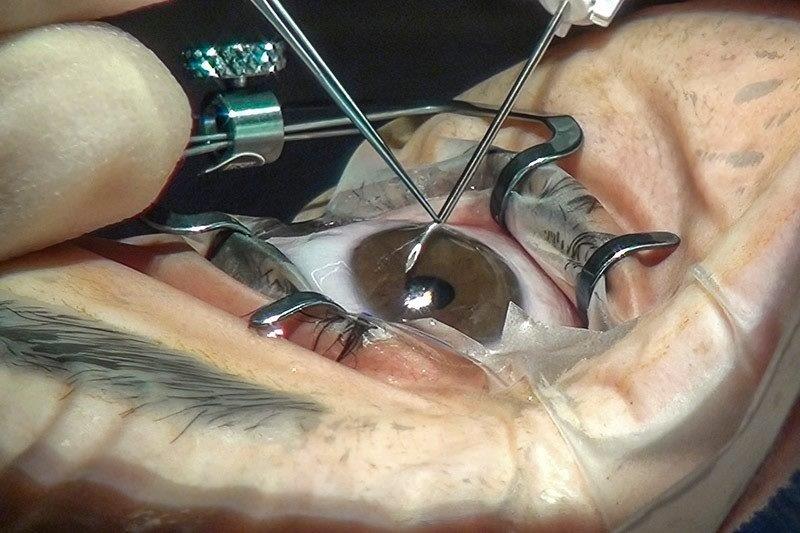
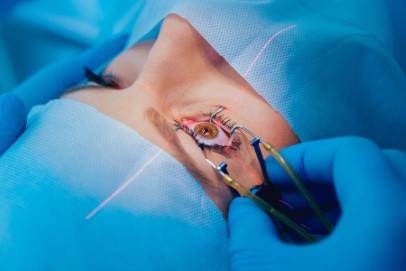
Among many excellent presentations, Dr Lynette Johns (Harvard Medical School, MA) and Dr Stephanie Woo (Havasu Eye Center, AZ) debated the ideal diameter of scleral lenses, with arguments for remaining less than 16mm including ease of handling, fewer issues with fogging and fewer problems with edge alignment. The use of larger diameters, beyond 18mm, conferred advantages of being able to vault the most diseased corneas, along with giving a larger, ‘softer’ landing area on the sclera. Ultimately, the advice was to own a fitting set of both a small and large diameter lens system, to understand the lens design and to select diameter based on the refraction and ocular surface needs of the patient.
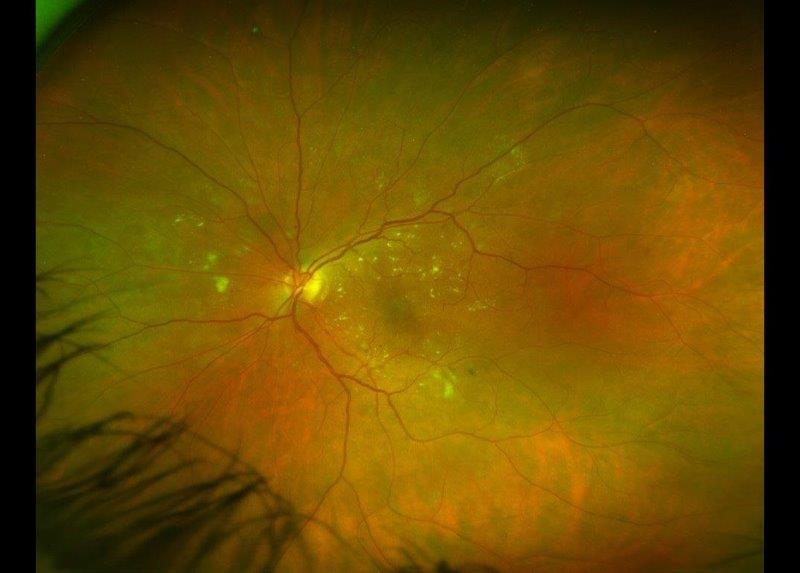
Dr Muriel Schornack (Mayo Clinic, College of Medicine, MN) and Dr Stephen Vincent (Queensland University of Technology, Aus) covered many of the aspects of scleral lens fitting that are not fully understood. These included the causes and clinical significance of transient physiological changes such as an irregular, “water-logged” appearance of the corneal epithelium (epithelial bogging) and perilimbal epithelial bullae. Dr Vincent shared some recently published work from his group which demonstrated the wide variation in lens profile and therefore in oxygen transmissibility between different lens designs. Corneal oedema peaks rapidly after around one hour of wear, he said, recovering very quickly within 30 minutes of lens removal. Both presenters commented on several aspects related to scleral lens wear that we still do not fully understand, such as the potential for altered intraocular pressure (IOP) with scleral lens wear and the lack of understanding of the effect of post-lens tear reservoir depth on oxygen transmission to the cornea.
Myopia control
Myopia control is a focus for practitioners at almost any educational conference these days, so it was no surprise that 11 hours of educational talks were dedicated to this very subject. Internationally renowned researchers and practitioners shared their knowledge and clinical expertise. Dr Maria Liu (UC Berkeley School of Optometry) gave a valuable presentation on pharmaceutical interventions for myopia control. Drugs which can target the posterior sclera are perhaps the most promising area of development, she said, while cautioning how challenging it is for a topically-applied agent to reach the intended site in these deep posterior tissues.
The non-specific nature of atropine’s anti-muscarinic blocking abilities means we still don’t understand the mechanism by which the drug slows myopia progression. Evidence shows both a dose-dependent response along with a larger rebound effect typically associated with higher concentrations. This means that a balance has to be struck, said Dr Liu, between efficacy and induced side-effects when thinking about the concentration to use, and while other agents such as pirenzepine and 7-methylxanthine are being investigated, currently, atropine is still the most likely agent to be used.
Dr Jeff Walline (Ohio State University, OH) and Dr Pauline Cho (Hong Kong Polytechnic University) covered existing evidence for the efficacy and use in practice of soft multifocals and spectacles for myopia control. When discussing efficacy with parents, Dr Walline pointed out study results give an average response, but it should be remembered that each child’s individual response may differ from that ‘average’ number. Mention was also made of spectacle lenses specially designed for myopia control, though the designs currently have little published evidence to support the claims.
Drs Liu, Cho and Vincent were joined by Patrick Caroline (Pacific University, OR) for a well-attended discussion on several aspects of myopia control. Dr Liu provided an overview of the complexities of study design within this field and the challenges associated with interpreting results. She also reminded us how difficult it is to truly run a double-blind trial, with cues for both patients and practitioners present in both ortho-k and atropine treatments.
Dr Cho discussed the results of a recent study from her group which examined the efficacy of ortho-k on the progression of both fast and slow progressing myopes. They found the rate of progression was relevant, with fast progressors producing good results with ortho-k after seven months, but slower progressors not showing a clinical benefit over the same time period. She suggested older children, above nine years of age, should be monitored for six months to establish their rate of progression prior to making a decision about starting ortho-k.
Pat Caroline then took the large audience on a deliberately thought-provoking journey in the last section of the session. Discussing power variation from the centre to the periphery of both contact lenses and spectacle lenses, he shared a series of graphs demonstrating that in the majority of cases, the peripheral power is higher than the centre. For example, depending on the lens design, a -3.00D contact lens increases in minus power at 6mm from the centre by 0.83D to 1.78D. This is obviously at odds with current theories exploring the benefits of imposing positive retinal defocus on the peripheral retina to slow eye growth. He called for more research into the optics of corrective lenses and it remains to be seen whether this theoretical mismatch translates to clinically-measurable differences.
Overall impression
GSLS 2019 was a vibrant conference, full of experienced, skilled practitioners keen to share their knowledge and learn new clinically-relevant information. I left with a surprisingly consistent feeling: the overriding sense that as we push the boundaries of our knowledge, we continually uncover things we do not know; questions we cannot answer, yet. This is ultimately a good message. It demonstrates that these technologies, and the practitioners who are using them, are at the cutting edge of patient care; pushing boundaries, using the best possible, most current evidenced-based approach, whilst being aware of the need to keep up to date with our continually-changing understanding of these challenging areas.
GSLS is a great environment to bring these practitioners, researchers and manufacturers together. I look forward to returning next year and learning more from my peers.
Karen Walsh is a clinical scientist at the Centre for Ocular Research & Education (CORE) at the University of Waterloo in Ontario, Canada. After graduating with first class honours in optometry from Cardiff University, Wales, she worked at practices in the UK before joining Johnson & Johnson Vision as professional affairs manager. She moved to Canada in 2015 and completed a two-year medical research fellowship. She is a fellow of the International Association of Contact Lens Educators and a high myope, so she knows the life changing benefits of contact lenses.