The lie that is soft contact lens ‘fitting’
For anyone who has followed these specialty contact lens articles over time you will have noticed a conspicuous lack of mention of the dominant segment of the contact lens market - soft lenses. The reason for this is simple - I don’t consider the fitting of modern soft contact lenses much of a specialty. In fact, many would argue that the term ‘fitting’ is inappropriate given the process generally involves unscientifically selecting a favourite lens type from a trial set and seeing how the patient goes with it.
Contrast this with fitting a rigid corneal lens. These days we are using an array of technologies to assess a cornea: its elevation, curvature, asphericity, irregularity and diameter. With this information we can then design all aspects of the lens: radii of curvatures, peripheral designs, edge profiles, size, thickness, material, surface treatments. All to generate a lens likely to provide optimum comfort, physiology and vision. And if for any reason during the process something is not quite right, then these parameters can be altered to one’s heart’s content. To me this is how contact lens fitting should be - for all lens types.
Eef van der Worp, a Dutch contact lens expert and educator, was one of the first to draw attention to the limits of modern soft contact lens fitting*. In a Contact Lens Spectrum article from November last year, Eef laments the challenge of teaching students soft contact lens fitting.
Cast your mind back to your university days. Conventional soft contact lens fitting principles involve adding a certain value (say 0.8mm) to the central keratometric data to determine the ideal starting lens. This is fine in theory but has the potential to frustrate a student when they learn that no readily available disposable lens with an 8.2mm BOZR exists. In these situations, the student must find the nearest possible option, somewhat undermining the strategy they have been taught. What then if the lens appears too loose and mobile? There may not be an alternative parameter in that material. Selecting and adjusting a lens based on corneal diameter is similarly flawed. Or as Eef puts it: “You can’t teach a student to believe in Santa Claus, only for them to find out in the real world that he does not exist!”
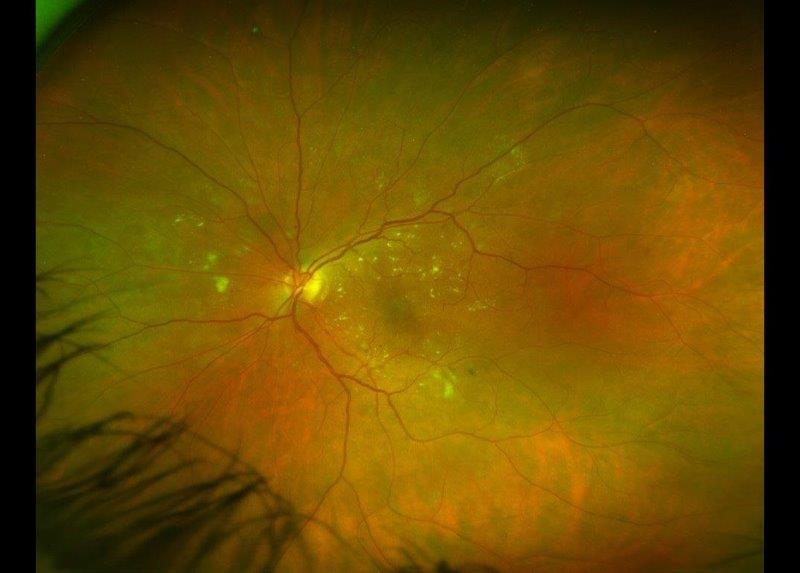
It is important to appreciate that there is considerable variation in shape and size of a normal eye. With the corneoscleral topographers that are now available such as the SMap and the Eye Surface Profiler, plus anterior OCT topographers, these ranges can be better understood. Several studies have shown that the average sagittal height of the cornea is around 3750 microns when measured at a 15mm chord. However, the spread of these measurements in normal eyes can vary 600 microns either side of this mean (Fig 1.).
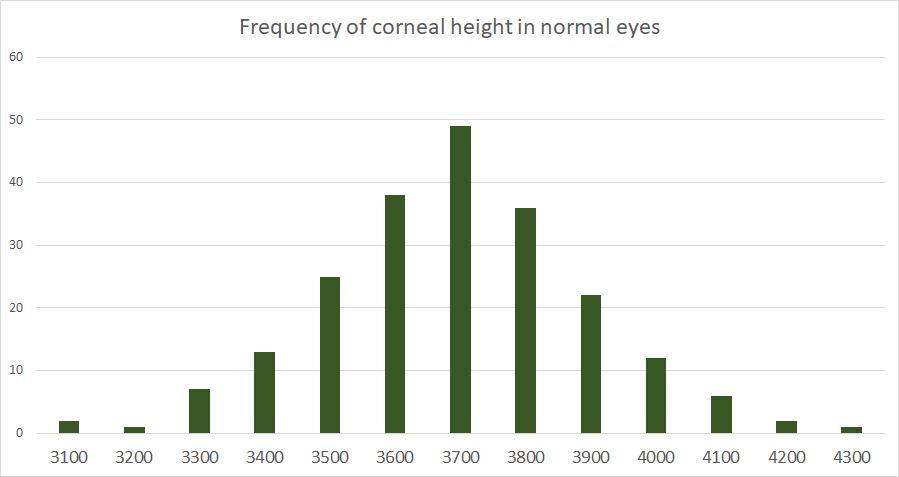
Fig. 1
The sagittal height of an eye is crucial in any contact lens fitting. It is relevant in soft contact lenses when we appreciate that the stated base curve of a lens and the lens diameter are really just surrogates for the sagittal height of the lens. Stapleton et al 2017 states that increasing sagittal height of the lens decreases lens movement and improves comfort. What this means is that it is principally the sagittal height change associated with altering the base curve or diameter of a soft lens that is actually changing the lens fit. Understanding this concept is a key part of improving how we think about soft lens fitting.
One of the problems I see is, as practitioners, we are not told any information about the sagittal height of commonly available soft lenses. So even if we can measure our patient’s corneal data, we cannot apply it in a scientific way. A recent study attempted to shed some light on this by measuring the contact lens sagittal height of common fortnightly and monthly replacement silicone hydrogels (Fig 2.).
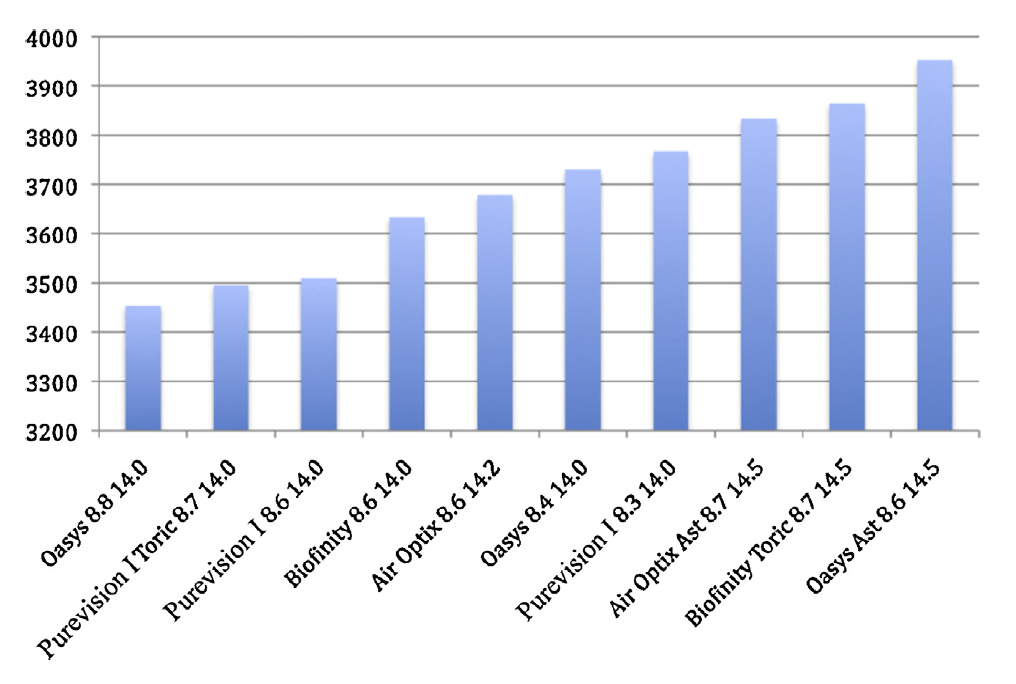
Fig. 2
As expected the steeper base curve lenses had a larger sagittal height for the same lens design. Importantly they found that the range of spherical lens sagittal heights to be only 330um across all designs; barely sufficient to accurately encompass the ~900micron range of normal eyes one would think.
Some interesting findings came out of the study too:
- There was up to 170 microns of sag variation between lens designs with the same base curve, meaning one 8.6mm lens cannot be simply exchanged for another of the same base curve;
- If a patient needs a lens to correct astigmatism, changing to the toric version of a lens design can add 500 microns for one lens design, and not alter the sagittal height at all for another.
In my mind, this confirms the limited use of the reported base curves and diameters on soft contact lenses. Instead remove the smoke and mirrors: why not just state the power and the lens sagittal height at an industry standard chord? We can then begin to better select the appropriate starting lens for a patient, know which lens to change to if an alteration is required and know when a patient is likely to need a custom soft lens to fit them appropriately.
A recent study from the UK looked at the success of fitting contact lenses and found that one year after fitting, 26% of patients had ceased wear. Of these, almost half dropped-out within two months. Incredibly about 70% had not been offered an alternative lens design or management strategy. We all know there are a range of complex reasons for contact lens dropout; comfort being only one of these factors. It is foolish to think matching sagittal height of a contact lens to an eye will solve all soft lens fitting problems as there are major differences that exist in lens material, roughness, friction forces and edge profile that affect comfort for patients. But if we can identify those patients for whom the narrow range of standard lens designs are not well suited, and instead use extended range or custom soft lens designs to optimally fit them, then it is likely that drop-out rates, especially for this cohort, will decrease.
A group of contact lens educators, including our friend Eef, met at the recent Global Contact Lens Symposium to plan a white paper: a multi-centre study to evaluate whether optimally aligning and confirming the shape of a soft lens with the shape of the ocular surface can make a difference in patients’ wear comfort to aid in reducing soft lens dropout. I await their findings with interest.
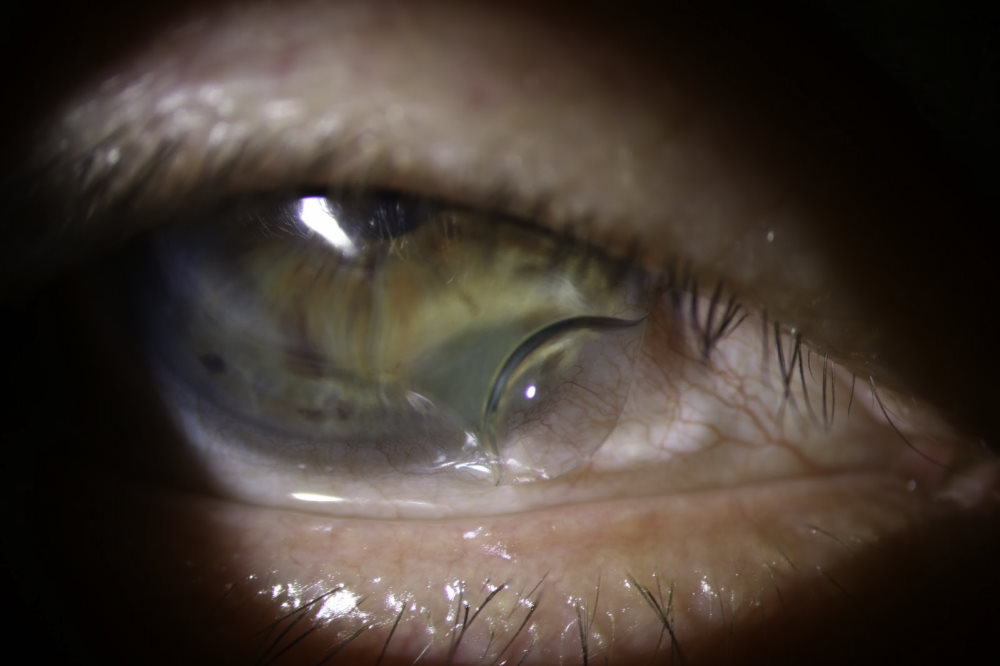
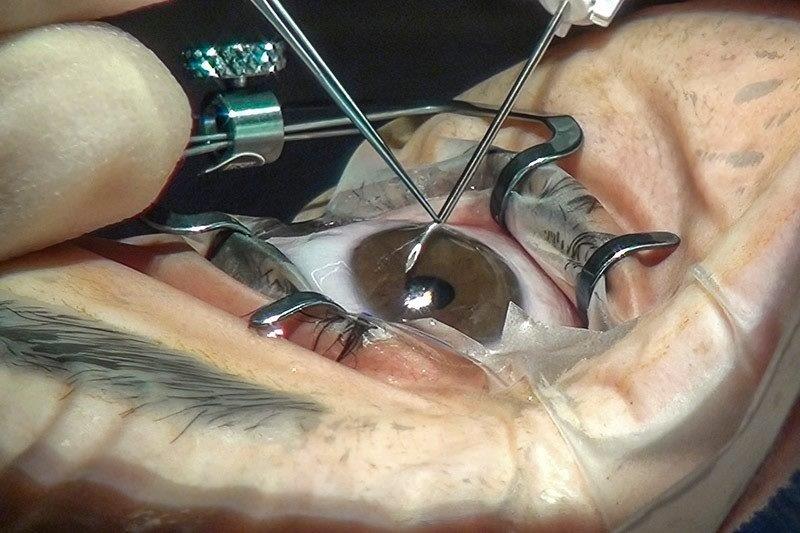
Fig. 3
To summarise: the current protocol for fitting soft lenses, involving central keratometry and base-curve selection, is misleading. You can’t measure a toe to determine shoe size. We need to be evaluating corneal shape and have the support from industry to support this fitting strategy. Hopefully, contact lens manufacturers will soon offer more tools and options to contact lens fitters to facilitate this paradigm shift of bringing back the ‘fitting’ to soft contact lenses.<
References
CL Spectrum Nov 2017. Data from Reinier Stortelder.
- van der Worp, C. Mertz / Contact Lens & Anterior Eye 38 (2015) 157–162
Sulley A et al 2017. Factors in the success of new contact lens wearers. Contact Lens & Anterior Eye
*Eef also pens a monthly email newsletter about specialty contact lenses called I-site, which I find invaluable to keep up to date with worldwide advances and research, sign up at www.netherlens.com.
About the author
Alex Petty (BOptom hons, FIAO) is a New Zealand optometrist based at Bay Eye Care in Tauranga, with a particular interest, knowledge and passion for specialty contact lenses, ortho-k and myopia control.