Myopia management applications
Myopia management has developed into a significant segment of clinical practice in recent years. Interventions primarily aim to attenuate the development of refractive error through the slowing of axial growth, either through pharmacological or optical mechanisms. While spectacle lenses represent a relatively immature branch of optical interventions, they are attractive in practice due to ease of implementation and the rapidity with which change or removal from the clinical strategy may be implemented1-3.
The two primary methods of monitoring the development of the paediatric eye are refractive error and biometric measurements. While both are powerful diagnostic tools, they are also lag indicators, which makes predictive modelling of emmetropisation something of a holy grail for myopia management. Standard eye-growth charts have some utility but can be limited due to growth variability from factors such as ethnicity and genetics, as well as external factors such as the dioptric complexity of the visual environment and existing refractive error correction as worn by the patient4. Consequently, the management of myopic progression is difficult from a predictive perspective, requiring continued and regular engagement with the patient to monitor their response to interventions.
Spectacle lens adaptations
Spectacle interventions are strongly directed away from single-vision lenses. The interaction between the far-point sphere (FPS) and the eye tends towards hyperopic defocus for single-vision lenses, which is implicated in the signalling for ocular growth and axial lengthening5-8. Multifocal designs have shown varying results, from low impact on axial lengthening for progressive addition lenses (PALs) to moderate for prism-control bifocals (in a relatively narrowly defined set of cases). The majority of current myopia control-lens designs aim to induce peripheral defocus to provide competing signals to eye growth. This is achieved through two main pathways:
- Physical surface geometry, ie. lenslets of increased power on the lens front surface inducing areas or volumes of defocus relative to the bulk of the lens surface. These lenslets may be consistent in power across the treatment area or modify radially. Common to both is the overall geometry of a central disc of distance prescription surrounded by a treatment zone in which the defocus is induced (Fig 1)9,10
- Freeform surface geometry, applied to a range of lens designs released over the last year which enable more complex interactions between the image plane and the asymmetric curvature of the retinal surface to be implemented (Fig 2)2
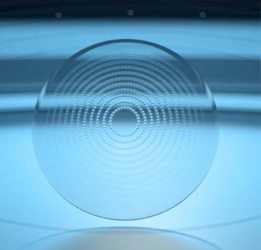
Fig 1
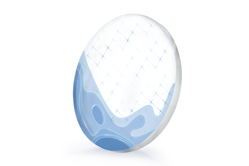
Fig 2
A notable exception to the defocus lenses is SightGlass Vision’s DOT 0.2 lens11, which induces areas of modified contrast rather than defocus. While the mechanism for myopia control differs from the above, the physical layout of the lens surface is similar to the radially symmetric defocus incorporated multiple segments (DIMS), used in Hoya’s Miyosmart lenses, and highly aspherical lenslet target (HALT) lenses, with a clear central disc and a treatment ring, in Essilor’s Stellest.
Fitting requirements
While spectacle lenses in this category tend to be aspheric, in many cases highly so, the physical properties of the surfaces present an obstacle to applying the centre of rotation rule to fitting. Designs with lenslets or physically defined surface geometry require the eye to be centred with respect to the treatment zone. This ensures that the area or volume of defocus is well placed on the retinal surface, thus enabling the design to work effectively. We know that the presence of pantoscopic tilt demands the dropping of the fitting height by 1mm per every 2 degrees of tilt, which may violate this fitting requirement. Note the relative shift of the size and angular relationship of the superior treatment zone to the inferior zone in Fig 3.
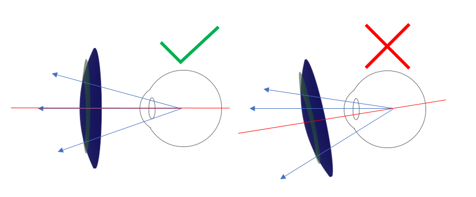
Fig 3
Designs using freeform surfaces may be considered to be closer in fitting modality to a progressive lens. In this way, the treatment zones are not readily visible to the practitioner, so we are more reliant on engravings and markings to ensure proper centration. As with progressive lenses, the relationship between the patient fitting and the layout of the lens is carefully considered at the design level, so the practitioner should refrain from applying any ad hoc changes to fitting heights. Attempting to drop or raise heights away from recommended fitting points risks negating the benefits of the lens. The requirements will vary according to design, but the general rule is to allow adequate lens to exist in each meridian to ensure the zones of defocus are in place (Fig 5). One example is:
- >5mm above pupil
- >12mm below pupil
- >12mm from frame (nasal)
- >25mm from frame (temporal)
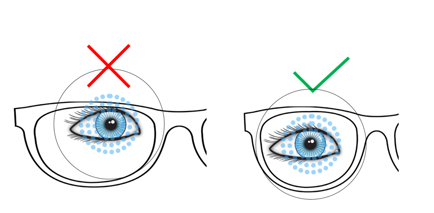
Fig 4
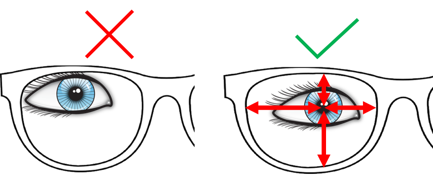
Fig 5
Of equal importance to the selection and fitting of the spectacle appliance is the long-term management of the patient. To effectively react to changes in the emmetropisation of the patient, it is important that practice staff work together to initiate and maintain compliance for both patient wear and follow-up consultations. Mapping of the roles of everyone in the patient plan and plotting the communication strategies are powerful tools in ensuring optimal outcomes. The most successful interventions are those where the team from the front desk through to the consult room and the lab are all clear on their role in the patient journey.
References
1. Cheng D, et al. Effect of bifocal and prismatic bifocal spectacles on myopia progression in children: three-year results of a randomized clinical trial. JAMA Ophthalmol. 2014;132(3):258–264.
2. GMBH R, Mycon by Rodenstock white paper. 2023.
3. Arias A, Artal P, Wahl S. Optical characterisation of spectacle lenses for myopia control. SPIE Optical Technologies. 2023. XXXII.
4. Harb E and Wildsoet C. Origins of refractive errors: environmental and genetic factors. Annu Rev Vis Sci. 2019 Sep 15;5:47-72.
5. Seidemann A, et al. Peripheral refractive errors in myopic, emmetropic, and hyperopic young subjects. J Opt Soc Am A Opt Image Sci Vis. 2002 Dec;19(12):2363-73.
6. Charman W and Radhakrishnan H. Peripheral refraction and the development of refractive error: a review. Ophthalmic Physiol Opt, 2010. 30(4): p321-38.
7. Tepelus T, et al. Effects of lenses with different power profiles on eye shape in chickens. Vision Res. 2012 Feb 1;54:12-9.
8. Atchison D. Peripheral refraction, peripheral eye length and retinal shape, in Optica Summer Data Blast. 2023, Optica: Washington DC/Online.
9. Maher C. Two year clinical study outcomes for the Defocus Incorporated Multiple Segments (DIMS) spectacle lens SUMMARY. 2021.
10. Li X, et al. Influence of lenslet configuration on short-term visual performance in myopia control spectacle lenses. Front Neurosci. 2021 May 25;15:667329.
11. Rappon J, et al. Control of myopia using diffusion optics spectacle lenses: 12-month results of a randomised controlled, efficacy and safety study (CYPRESS). Br J Ophthalmol, 2022.

Grant Hannaford is a senior lecturer at the School of Optometry and Vision Science UNSW, the past-chair of the NSW Optical Dispensers Education Trust and the past-vice president of ADOA (NSW). A co-founder and director of the Academy of Advanced Ophthalmic Optics, he co-owns Hannaford Eyewear and was 2022’s Silmo IOA International Optician of the Year. Australia’s first qualified spectacle lens designer, Hannaford is a doctoral candidate at Aston University, UK, where he’s researching emmetropisation and ocular biometric development in children.



























