Inspiration and collaboration with AONAWA
Running alongside the Saturday of the RANZCO 2023 conference at The Perth Convention and Exhibition Centre, located beside the majestic Swan River, was the Australian Ophthalmic Nurses Association Western Australia (AONAWA) 2023 meeting, aimed at all the region's ophthalmic nurses.
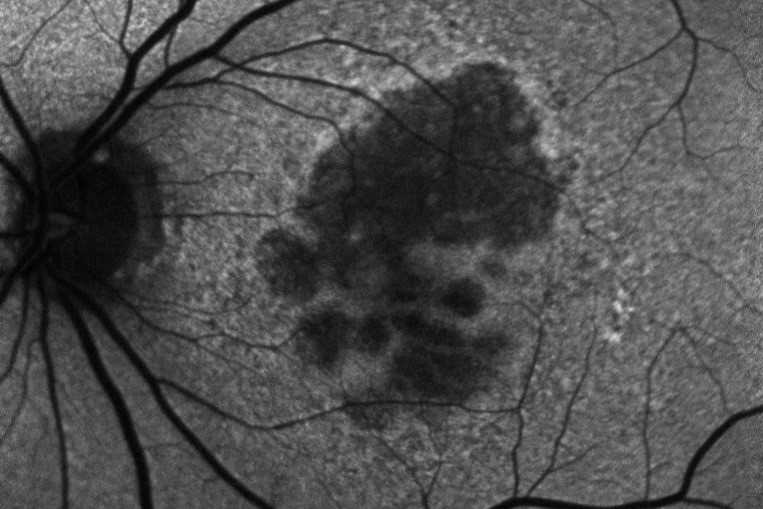
The University of Western Australia’s Dr Fred Chen launched us into the day’s programme with a discussion on the pathophysiology of age-related macular degeneration (AMD) and his research on faricimab (Vabysmo), the latest treatment for wet AMD, macular oedema and vitreous haemorrhage. Faricimab boasts a longer time between treatments compared with aflibercept (Eylea) and a similar safety profile. It’s now available in Australia, but not yet in New Zealand. There was some scepticism around the length of treatment extension suggested by the manufacturer, however, so watch this space.
Oculoplastics surgeon Dr Pav Gounder’s presentation of various case studies was fantastic. It included the usual gruesome surgical photos we all love to see, but with great postoperative results. He emphasised the value of a multidisciplinary procedural approach and gave an example of an impressively sized rotational flap with the aid of ENT and head and neck specialists. He also described a case requiring orbital decompression surgery for thyroid eye disease, using scopes for viewing orbital sinuses, which was fascinating.
Next was the inspirational and entertaining Dr Scott Hollier, CEO and co-founder of the Centre For Accessibility Australia, who described his experience after being diagnosed with retinitis pigmentosa (RP), aged five. He highlighted how important it was for health professionals not to deliver a dismal prognosis for a sight-threatening diagnosis, explaining how his experience with a second doctor’s positive and optimistic opinion set him on the right track to live a productive, fulfilling and successful life. An e-copy of his autobiography was given to conference attendees and New Zealand nurse Ashleigh Malcolm was lucky enough to win a hard copy! Dr Hollier explained how apps and voice-command technology for the visually impaired have helped him tremendously. This included ‘Be My Eyes’, an app which allows users to point their phone camera at something, so a sighted volunteer connected via the app can describe to them what it is. It sounded fantastic!

The Perth Convention and Exhibition Centre, host to RANZCO 2023 and the Australian Ophthalmic Nurses Association meeting
Isolated eyecare
Nurse practitioner (NP) Liz Oakley shared her experience as the only eyecare professional serving Thursday Island’s population of 2,805. Although an optometrist and ophthalmologist visit the remote Torres Strait island two to three times a year, Oakley lives there, screening for diabetes and glaucoma and performing vision checks in schools. Her work is varied but is inhibited due to a limited scope of practice, which seems typical for Australia’s ophthalmology nurses. Unfortunately, Medicare (and RANZCO) restrictions mean NPs in ophthalmology can’t practice autonomously, as they do in New Zealand, regardless of need. An example of this is the limited list of ophthalmic medications Oakley can prescribe, which, amazingly, does not even include IOP-lowering drops!
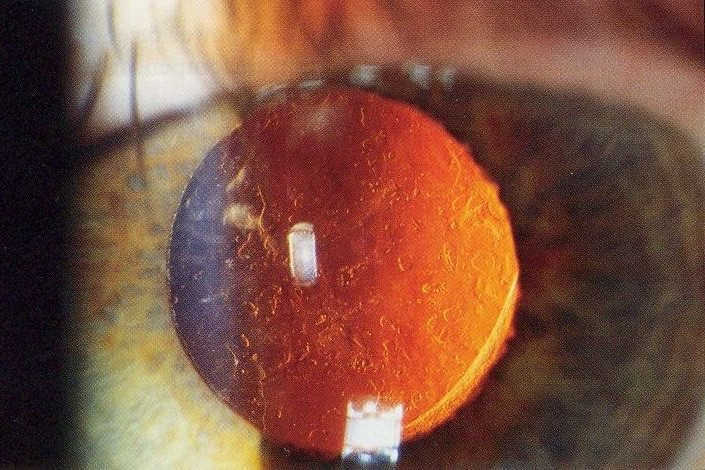
RN Peter Mitchell spoke of his rewarding role in a vanguard team of travelling eyecare professionals. Consisting of himself, a theatre nurse, an orthoptist, an optometrist, an anaesthetist and an ophthalmologist, the team provides cataract surgery to patients in remote areas of Australia. Mitchell also discussed his involvement in Cambodia Vision and overcoming the difficulties of access to care there.
Continuing the theme of helping Australia's more isolated communities, Lions Outback Vision’s Dr Yachana Shah’s talk on outback teleophthalmology services explained Western Australia’s access to care challenges, due to the vast distances between populations and limited availability of ophthalmologists and optometrists. She explained that teleophthalmology is cost-effective and collaborative care with GPs and optometrists is now making this model of care much more common. Just three ophthalmologists in the city of Broome cover much of the northern area of Western Australia, providing an on-call service to Kimberley’s 419,558km² – twice the size of Victoria. They support the region’s 36,000-plus people, who are spread between six major townships and more than 160 small, remote Indigenous communities; 50% of the population is Aboriginal, with over 30 traditional languages spoken. The remoteness of some of these outback towns means some patients travel 30 hours or more to receive acute surgical specialty care in Perth.
Crosslinking, nerves and nursing concerns
Ophthalmologist Dr Ulrike Schrifl was excited to present on their new crosslinking service for keratoconus patients in Fremantle, which commenced in June 2023. It was surprising, however, that this was a new service, as New Zealand has been providing this for quite some time with nurses performing the procedure for well over a decade.
Known online as ‘The Breakthrough Nurse’, Hannah Sawyer discussed the pressures of nursing and the negative impact it can have on our nervous system. As nurses, we tend to over-give and have a lot of unprocessed, suppressed emotions, so she took us through some breathing exercises to help with stress relief. I would imagine her service is in high demand!
Presenting her research into the Australian ophthalmic nursing workforce, RN Dr Heather Machin said the workforce is dwindling alarmingly, with more than 68% of eye nurses stating their intention to leave the profession within the next five to 10 years. She highlighted nurses' invisibility in the 2009 and 2016 Vision 2020 documents, which focus on service delivery, workforce and training, preventative healthcare, equity and sustainability. She was concerned about the seeming lack of recognition for Australian ophthalmic nurses as integral members of the eye workforce in these key areas.
I presented on implementing nurse-led clinics. Unfortunately, this is also a rarity in Australia, with only two nurses in the audience leading their own eye clinics and no apparent opportunities for nurse-led clinics in the workplaces of the other nurses present, with most saying they work in private care. This was another reminder of how New Zealand is extremely fortunate to have a health system which allows the development of advanced ophthalmic nurse roles and embraces nurse-led clinics to increase access to timely, effective and cost-effective patient care. Nurses are not utilised in Australia as they are in New Zealand, but despite playing a key role in the delivery of care, New Zealand nurses also remain mostly invisible when it comes to formal recognition. I came away not only feeling that ophthalmic nurses in Australia and their skills need to be recognised and utilised more, but also that nurses in Aotearoa need a stronger voice and profile in New Zealand’s ophthalmic community. Since we care for our patients as much as any other eyecare professional, we should be involved in national and international decisions regarding the provision of their care. Perhaps a solution would be to become affiliated with RANZCO, so nurses can be actively involved in the future direction of ophthalmic care. After some positive discussion in Perth, this option is currently being looked into. I will share any future developments with my New Zealand colleagues as they come to hand.
Overall, both the RANZCO and AONA conferences were enjoyable, informative and set in a wonderful city. It was pleasing to know our community is delivering an extremely high standard of care. However, we face the same challenges as Australia with increasing patient numbers and a workforce that cannot keep up, but at least in New Zealand nurses have the tools and support needed to help fight the backlog.
Fiona Bamforth is a nurse practitioner with more than 30 years’ experience in ophthalmology in the UK and New Zealand. She practices privately in Whangarei and Nelson and publicly in Nelson and in Westport.