Pearls in Perth – the 54th annual RANZCO conference
I had the privilege of attending the 54th annual RANZCO meeting in Perth, the ancient country of the Whadjuk Noongar people, the traditional owners of Western Australia’s southwest. The event brought together not just some of the brightest minds and leaders in the ‘meeyal’ (eye) field, it was also a dynamic platform where knowledge, innovation, and collegiality intersected to shape the future of our vocation.
At the opening ceremony, Professor Leonard Collard formally welcomed us in several languages to the sound of a didgeridoo. Dr Craig Challen then held the audience in awe as he described his role in the rescue of 13 young Thai boys trapped in the Tham Luang cave in 2018. Each of the boys, many of whom couldn’t swim, had to be kept sedated for more than 30 minutes by a team of mainly non-medical cave diving specialists as they were individually swum out through the winding, flooded cave system. Dr Challen’s concluding thought was his belief that everyone faces a test at least once in their lifetime, for which they were in a way unprepared, but which they had also been preparing for their whole life. He showed our experiences outside our careers build our resilience, strength, competencies and knowledge, which in turn help in many aspects of our lives both professionally and personally.

Dr Craig Challen, Australian vet and cave diver, captivated the RANZCO 2023 audience with his
opening address about his role in the Tham Luang cave rescue
Improving eyecare equity globally
The Global Eye Health Workshop had speakers from New Zealand, Australia, Samoa, Fiji, Papua New Guinea, Indonesia, Bali, Cambodia, Singapore and India. This session highlighted the need for global action and to keep equity, access, quality and affordability in mind while expanding the ophthalmic field. The vast inequality in access to healthcare was brought to light by Central Australia’s only ophthalmologist Dr Tim Henderson’s interesting discussion with Flinders University uveitis and ocular parasite specialist Professor Justin Smith on ‘fly-in, fly-out’ medicine. Between the two of them, they provide cover for a rural Australian area the size of Spain! To increase healthcare access, they have introduced rural satellite offices and book out weekly clinics, a practice similar to Aravind Eye Hospitals, India’s network of ‘affordable eyecare’ hospitals, which has now established a network of satellite clinics to improve retinopathy of prematurity (ROP) screening and awareness to keep pace with the high number of premature births. Dr Henderson said his experience is that in some remote communities, positive learnings are not always passed down the generations as strongly as the negative learnings are, which explains why healthcare provision isn’t always taken up by communities. It was also highlighted that since dialects and languages are a key barrier to healthcare access, it’s crucial to work with and train local people.
These topics informed RANZCO’s Vision 2030 goals, which were discussed by Dr Kristin Bell from the Royal Hobart Hospital, Tasmania. She highlighted the growing cost of healthcare versus the stagnant funding of eye healthcare, emphasising that trainee numbers are not sufficient for sustainable provision of and investment in preventative medicine. Dr Justin Mora, chair of the RANZCO Māori and Pasifika Eye Health Committee and clinical lead of Vision 2030 Aotearoa, then provided an update of RANZCO’s vision aspirations in New Zealand. This included some positives, such as the gains made in cataract funding provision (though few details have been released of how this will eventuate) and more support for low-vision care, and some negatives: the lack of optometry support in more remote regional areas and any sort of national eyecare survey or plan.

Dr Justin Mora and RANZCO NZ chair Dr Liz Insull
AI: positives and negatives
Another thought-provoking theme was whether artificial intelligence (AI) is the great equalizer or the great divider! With increasing technologies and better treatment options, it’s important not to leave those less fortunate or less able behind.
University College London and Moorfields’ head of artificial medical intelligence Professor Pearse Keane’s presentation focused on using AI to reduce the burden on outpatient clinics, for example, to triage patients from their OCT scans. He also shared news of the Insight Research Hub for Eye Health, an NHS-developed cloud-based research resource, loaded with 22 million pictures and extensive data, such as the numbers of injections patients have received tracked against their visual acuities. It is updated daily and since it’s open source, it can be used globally for research by anyone! Prof Pearse, together with visiting ophthalmologists from India’s Aravind Eye Hospitals, discussed some of the incredible benefits of combining AI and telehealth in a separate session. These were also key themes in Lions Eye Institute Associate Professor Angus Turner’s post-RANZCO satellite meeting in Broome, which was designed to show how these new tools could significantly help impoverished populations, such as Australia’s Indigenous community.

Drs Kenneth Chan, Antony Suter and Yu-Chieh Hung
Pearls galore
There was no shortage of pearls from all subspecialties across the three-day conference. These were some of my notable take-homes.
Eyelids
Dr Jo Richards (Perth) reminded us that rosacea is mostly triggered by the sun, but it can also be triggered by medications, especially prednisolone. Although it can affect all parts of the eye, patients will often present with atopy, other autoimmune diseases, metabolic syndrome, anxiety or type-2 diabetes. The bottom line was to give doxycycline (a great anti-inflammatory as well as an antibiotic) 50mg twice daily for one month, dropping to 50mg once daily for two more months. If the patient is not keen on this option, topical Soolantra (ivermectin) applied to the face at night (on five different spots, ie. above each eyebrow, between eyebrows and below each eye) for four months, is a good alternative.
Glaucoma
Professor Tina Wong, head of the Ocular Therapeutics and Drug Delivery Research Group at the Singapore Eye Research Institute, advocated for ibuprofen 400mg three times daily for one-week post operatively as it reduces the likelihood of bleb failure and intraocular pressure (IOP) increase by reducing collagen crosslinking. A combination of valproic acid and reduced mitomycin-c dosage can be used to modulate collagen architecture and retain more normal vasculature. She also covered drug-eluting implants such as iDose (travoprost placed in the trabecular meshwork).
Cornea
Descemet's membrane endothelial keratoplasty (DMEK) and Descemet's stripping automated endothelial keratoplasty (DSAEK) result in a postoperative hyperopic shift. Therefore, according to Associate Professor Elaine Chong (Melbourne), we should aim for -0.5D to -1D. Another consideration, when Fuchs’ endothelial dystrophy hasn’t been diagnosed pre-operatively and a hydrophilic lens is used, is the potential issues when using air for DMEK as this will interact with the lens and can cause irreversible opacification.
Laser blended vision (Presbyond) leaves micro anisometropia in a blend zone of +0.75D in one eye and -0.75D in the other when using LASIK. It was noted LASIK is safe, accurate, centred over the visual axis, with high patient satisfaction, and no contrast loss. It is also reversible with glasses, and a monofocal IOL can be subsequently implanted. However, SMILE laser has less aberration than LASIK and causes fewer dry-eye symptoms as it is done below the nerve plexus, maintaining more tensile strength. We also learnt that cultured human corneal endothelial cell (CHCEC) transplants via injection have been proving effective in recent studies and implantable collamer lens sizing should now use ciliary body inner diameter, as opposed to sulcus-to-sulcus, as values can be up to 17% larger. There is a free formula available for this at www.iclsizing.com.
Cataract
Bilateral cataract surgery was touched on by several speakers. Overall, the view was that it’s now preferred by most patients and is more beneficial in terms of less wastage, fewer clinic appointments and less time wasted for patients and clinic staff.

Drs Mo Ziaei, Judy Ku and Elsie Chan
Uveitis
Whole sessions were dedicated to uveitis investigation, management and access levels in different countries. It was interesting to learn how useful immune suppression can be, with Professor Justine Smith and Dr Jo Richards both encouraging us to form good networks with rheumatologists and immunologists to ensure we feel comfortable starting these medications.
Dr Rachael Niederer (Auckland) shared a great talk on syphilis resurgence in Aotearoa, compounded by lower screening rates during Covid. When the diagnosis is unclear, even when YAWS (chronic bacterial infections) is suspected, it is crucial to treat patients as syphilis sufferers in order to maintain a safe practice.
Vitreoretinal
Phaco-vitrectomy for epiretinal membranes using non-expansile gas does not require any IOL power change. When using expansile gas for retinal detachment and macular hole, a power of +0.5D needs to be added or to aim for the first +. Using silicone adds 2D difference. IOL calculations also need to account for changes in axial length due to scleral buckling as it causes a myopic shift, and it is advisable to wait at least three months before doing a post-scleral buckle biometry. Another recommendation was to use a fourth-generation formula, such as Barrett Universal, Kane or EVO, as things have moved on significantly over the years.

Sylvia Hewison and Drs Anne-Marie Yardley and Chris Murphy
Retina
Faricimab (Vabysmo) is a new neovascular age-related macular degeneration drug whose benefits include lower rates of lesion activity, longer treatment intervals and stable visual acuity.
It was striking to hear diabetics are 2.6 times more likely to have diabetic retinopathy (DR) if they are Indigenous. We reviewed the latest landmark studies, including Yosemite, Rhine and Photon. Yosemite and Rhine compared faricimab and aflibercept in diabetic macular oedema (DMO) patients. It demonstrated that faricimab administered at eight- and at 16-week intervals was not inferior and provided good visual improvement compared with aflibercept administered every eight weeks. This could mean fewer clinic visits and decreased treatment burden. It also showed improved anatomic outcomes in previous non-responders.
Regeneron’s Photon study compared normal eight-weekly aflibercept versus high-dose aflibercept (12-weekly and 16-weekly dosing regimens). Results published in 2023 showed high-dose aflibercept was non-inferior to normal dose at eight weeks (in both dosing regimens) and could be extended out to 24-weekly doses with continued non-inferior mean BCVA at two years. Again, this could mean fewer visits, decreased treatment burden and better patient compliance.
DR in pregnancy was another notable topic. Although this condition needs to be corrected as quickly as possible for the mother’s and the child’s health, we know worse visual outcomes tend to result from quicker corrections. Post-partum, mothers usually stay the same or progress, but they don’t tend to regress. This is especially true if their systolic blood pressure is above 120mmHg in early pregnancy. The new recommendation for screening and follow-up is an eye clinic review during the first trimester. If DR is found, the mother should have an exam each trimester or as indicated by the clinician. In the case of no DR and type-1 diabetes, they should have another exam during the pregnancy; if there is no DR and type-2 diabetes, they do not require further exam during pregnancy. We still do not know what the best management is if a woman develops DMO during pregnancy, however. Associate Professor Lyndell Lim, head of the Clinical Trials Research Centre at CERA, is currently recruiting such patients, should you encounter any.

Drs Natalie Allen, Hannah Ng and Dan Scott
Neuro-ophthalmology
This year’s conference included an epic session on neuro-ophthalmology, hosted by Professors Helen Danesh-Meyer, Celia Chen and Neil Miller, who took us through a series of fascinating cases. My take-home messages were the following: if a young patient presents with a central retinal artery occlusion, we should always consider cardiogenic and thrombogenic causes; and a handy low-tech tip to help diagnose anhidrosis in Horner syndrome is to slide the back of a spoon across a patient’s forehead, as it won't glide easily with no perspiration.
When dealing with possible idiopathic intracranial hypertension (IIH) it is important to request magnetic resonance venography (or computed tomography venography) as well as a lumbar puncture. If a patient is diagnosed with IIH by exclusion but does not experience any headaches and shows only mild papilloedema, no treatment is required. If they have a mild headache and mild papilloedema, analgesia is sufficient. To reduce IOP, acetazolamide should be started at a dose of 1g per day in divided doses and can be titrated up to 4g per day safely. Acetazolamide has also been shown to help with weight loss, as have medications including topiramate and newer GLP-1 receptor agonists. These have been shown to work in non-diabetic patients too.
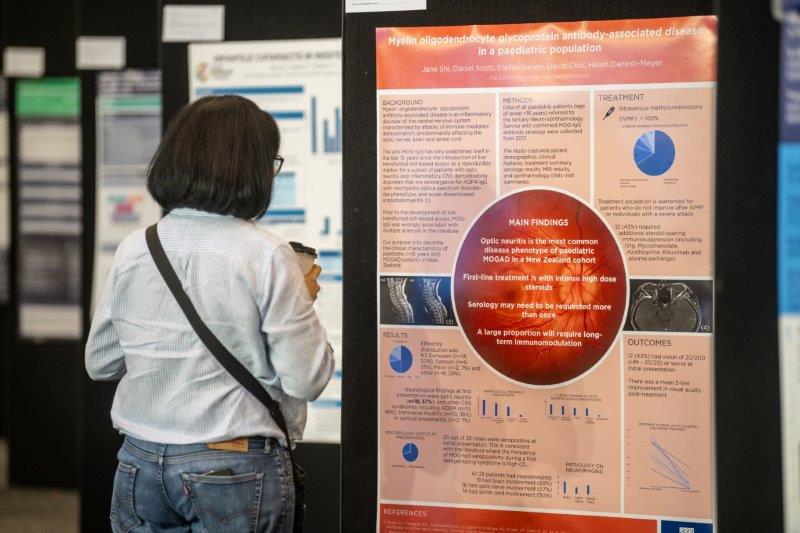
In cases of suspected optic neuritis, it is important to: check for neuromyelitis optica (NMO) via aquaporine-4 (AQP4) and myelin oligodendrocyte glycoprotein (MOG) antibody disease via anti-MOG antibodies; request an MRI; and treat all patients with methylprednisolone unless there’s evidence of intercurrent infection. It can be given orally (1,000mg for three days) if there is no IV availability. It is also recommended to give plasma exchange (PLEX), four to six months of steroids and an immune modulator if it is found to be MOG-related. Plasma exchange should be initiated if there is no improvement within seven days of treatment without waiting for antibody results. CRION (chronic relapsing inflammatory optic neuropathy) is in fact MOG-antibody-positive optic neuritis and these patients will require long-term immunosuppression.
In conclusion
New Zealand was well represented with many posters and session contributors, which was a pleasure to see.
Unfortunately, I missed out on the meditation, hula hoop and bike sessions as they all occurred at the same time as the breakfast sessions. Equally valuable sessions occurring at the same time was the event’s biggest downside. However, this is a common issue among large conferences of this type. That said, I felt the organisers did a wonderful job and the sessions ran smoothly. The sustainability station, where we could wash our free Rayner-sponsored reusable drink cups, was a lovely touch. In the same spirit, I noticed fewer objects and pamphlets being handed out.
Overall, this year’s RANZCO conference was an outstanding experience, serving as a positive reminder that in our interconnected world, collaboration and shared knowledge are key to progress. I eagerly anticipate the 55th RANZCO Annual Scientific Congress in Adelaide, from 1-4 November 2024, where we will continue to learn, share and shape the future together.

Dr Madelyne Jouart with Abbvie's Phil McNamara and Darrin Tommy
Dr Madelyne Jouart is a non- training registrar at Taranaki Eye Centre.