An eye on understanding our lifestyle choices
Recognising that everyday activities and exposures risk unintended consequences on the ocular surface was the driver behind the Tear Film and Ocular Surface Society’s (TFOS’) latest workshop. The TFOS Lifestyle Workshop, led by Professors Jennifer Craig (chair, New Zealand) and Monica Alves (vice-chair, Brazil) and Associate Professor David Sullivan (organiser, USA), involved 158 experts from 38 countries¹. Eight subcommittees generated topic area reports tackling relevant aspects of modern lifestyle. Three additional subcommittees provided further support across the breadth of the workshop on evidence quality, industry liaison and public awareness. The Evidence Quality subcommittee (a new initiative in this TFOS workshop) was tasked with promoting inclusion of relevant, high-quality evidence in the narrative review and reduced emphasis on outcomes from poorer quality evidence². This subcommittee’s members also led a systematic review within each topic to answer a key clinical question in the final reports.
An overview of each follows, sharing some of the latest evidence-based recommendations, including lifestyle factors to watch out for in patient interactions. It is important to note that the current literature doesn’t give us all the answers at this point. An important objective of the TFOS reports is also to highlight areas where knowledge is presently lacking to help direct future research.
Contact lenses
Contact lenses (CLs) improve quality of life for millions across the world but appreciating how wear choices can impact safety and performance is important³. Comfort and vision are reduced with non-adherence to scheduled replacement, which is especially concerning for daily disposable lens wearers untrained in safe overnight lens storage practices. Sleeping in contact lenses remains the single largest risk factor for microbial keratitis, along with topping off solutions, failing to regularly clean and replace cases and exposing lenses to tap water.
Daily disposable lenses enjoy the lowest complication rate and highest compliance levels of all wear modalities and are rated top by patients for convenience. Their disposal has potential environmental impacts though, so find out the appropriate local disposal and recycling options for contact lenses, packaging and care products to advise your patients.
CL choices that patients make can similarly impact performance. Purchasing lenses from unregulated outlets and lack of ongoing care increases risks. Wear may also be more complicated for those with systemic diseases with ocular surface manifestations such as diabetes, but ocular allergy sufferers may benefit from the physical barrier contact lenses provide, reducing ocular surface exposure to airborne allergens. Adverse environmental factors such as high altitude, low humidity, wind and pollution, as well as smoking and vaping can adversely impact contact lens success, so may also be worthy of discussion with patients.
Cosmetics
The lack of regulation of cosmetic products globally is concerning⁴. Laboratory testing shows that specific ingredients within cosmetics are toxic to cells, even when applied in quantities much lower than those permitted in cosmetics. Benzalkonium chloride is a well-recognised culprit that is still often present in cosmetics, potentially placing cosmetic-wearing patients at risk. Parabens and phthalates also risk adversely impacting the surface as they are endocrine disruptors. Anti-androgen activity within compounds designed to be applied on or close to the eyes is a risk factor for dry eye, so practitioners need to be alert to this.
Eye cosmetic procedures can also place the ocular surface at risk of harm, such as eyelash curling, perming, tinting and extensions. The use of glue and tape to create the appearance of an eyelid crease is popular in Asia but risks direct and indirect harm to the ocular surface, while procedures performed to rejuvenate the periocular skin are associated with a range of side-effects that warrant caution.
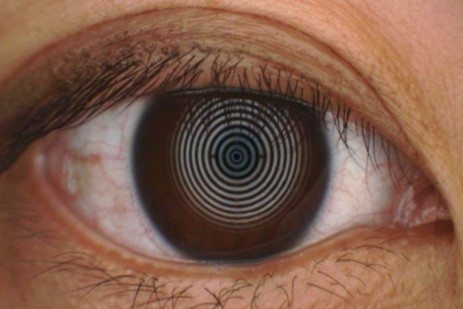
Digital environment
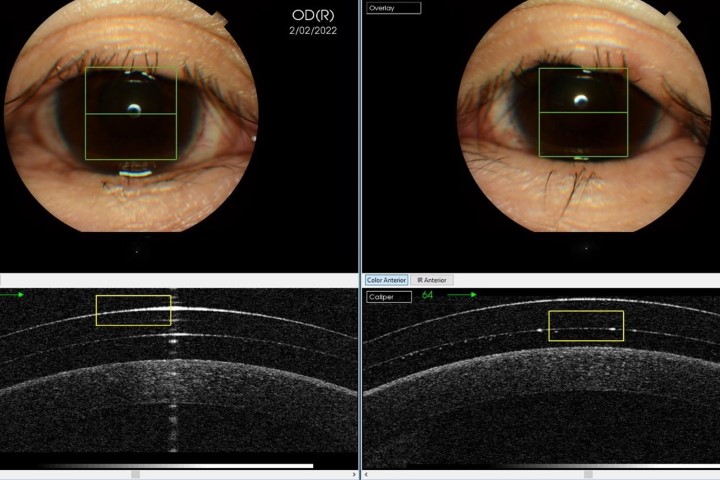
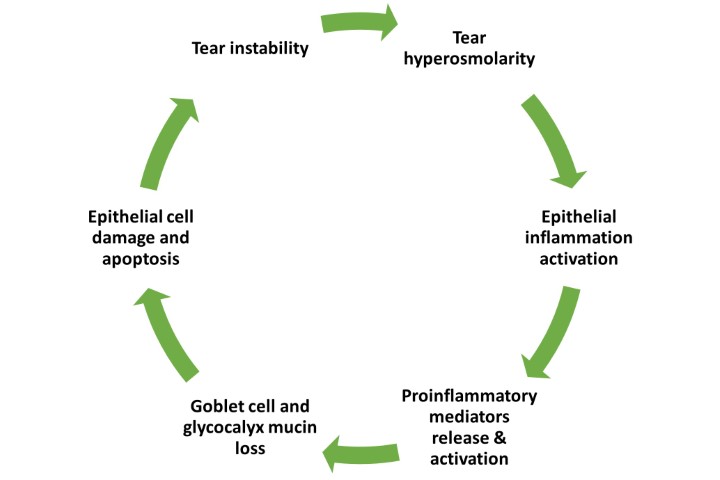
Exposure to the digital environment is close to unavoidable nowadays but can result in discomfort that worsens with increased time spent viewing digital devices⁵. Digital eye strain (DES) is the preferred term to describe ocular discomfort associated with digital viewing. With a high global prevalence of around 70%, the TFOS report warns that it’s important to differentiate DES from other underlying symptomatic conditions as being the development or exacerbation of ocular symptoms or signs during digital device use for a cognitive task, that doesn’t occur with an equivalent non-digital task.
DES symptoms vary according to whether the source is refractive/accommodative (blurred vision, focusing difficulties, eyestrain), ergonomic (neck and back pain) or ocular surface/dry eye-related (dryness, burning and irritation). The main mechanism attributed to dryness symptoms is reduced blink rate and completeness.
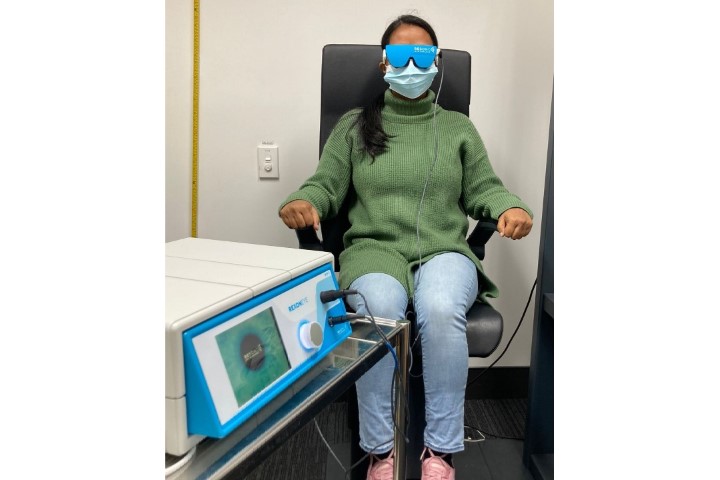
A multipronged approach to address refractive error, accommodative anomalies and ergonomics, as well as managing ocular surface and dryness issues, is recommended. Evaluation of the current best evidence on intervention practices showed omega-3 fatty acid supplementation had the clearest benefits, while local humidification and limiting daily screen use to 4-5 hours showed probable benefit, as did eyelid warming and reading from e-paper rather than screen. Conversely, blue-light blocking interventions and antioxidant supplements were found to be ineffective in relieving symptoms of DES, so should be avoided as recommendations to patients.
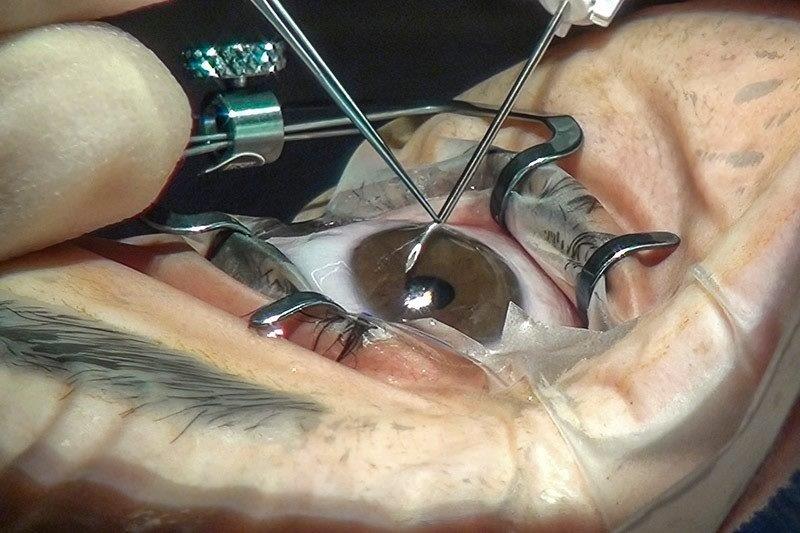
Elective medications and procedures
Patients often choose to take non-prescribed ‘over-the-counter’ products and undergo procedures for perceived health benefits or improved quality of life, but these products and procedures can have unintended ocular surface consequences⁶. Evidence describing the risks of artificial and natural products applied topically, whether as drops, gels or ointments, including those applied to the periocular region, are described. These include eyelid hygiene products, warm compresses, sunscreens, topical steroids and other creams and ointments. Impacts on the ocular surface from systemic medications were also evaluated, including isotretinoin, which risks damage to the meibomian glands, and hormonal therapies associated with dry eye disease.
Ophthalmic surgical procedures also have potential to compromise ocular surface health, resulting in iatrogenic dry eye disease and inflammation by impacting the nerves. The evidence, reviewed systematically, shows a lesser impact of small incision lenticule extraction (SMILE) on ocular surface nerves than conventional laser refractive surgery by avoiding creation of a corneal flap.
The risks associated with periocular cosmetic surgery and non-surgical procedures, which depend on the site, technique and quantity of tissue removed, are also acknowledged, as are preoperative risk factors.
Environmental conditions
Climate and pollution-related environmental factors including temperature, humidity, ultraviolet (UV) light exposure, pollutants and allergens have documented adverse impacts on eye health⁷. High temperatures, low humidity and rapid wind speeds disrupt ocular surface homeostasis. High altitude and UV exposure are linked with pterygium, ocular surface degenerative conditions and neoplastic disease, while pollution is associated predominantly with dry eye disease and conjunctivitis.
Nine percent of the global population lives within an active volcanic eruption zone, presenting a risk of keratoconjunctival foreign bodies and eye irritation. Indoor pollution, ‘sick-building syndrome’ and ‘sick-house syndrome’ have also been associated with eye irritation.
A systematic review considered evidence for associations between outdoor pollution and signs or symptoms of dry eye disease and found that dry eye disease is associated with air pollution (from NO2) and soil pollution (from chromium), but not from air pollution from CO or PM10 (particulate matter). Increasing awareness about potential impacts of environmental conditions, especially the modifiable components, may equip patients with valuable knowledge for tackling ocular surface disease.
Lifestyle challenges
Lifestyle challenges on ocular surface disease are subdivided into mental health, physical and social factors⁸. Different studies, across multiple geographies and populations, have identified relationships between mental health indices, such as depression, anxiety and stress, and dry eye disease, with the link being stronger for symptoms than for signs. Identifying and referring dry eye patients who might benefit from professional mental health support is important when managing patients with dry eye disease.
Obesity is a physical factor found to be linked to meibomian gland alterations. It is compounded by the association with sleep apnoea and related overnight use of continuous positive airway pressure (CPAP) devices. Face masks are a newly identified risk factor, with their impact related to daily hours of wear and number of months of use. Through systematic review, the evidence, although graded low in quality, was found to support co-morbidity between chronic pain syndromes (migraine, fibromyalgia, irritable bowel and back pain) and symptoms of dry eye disease.
Social factors such as tobacco, cannabis, other recreational drugs and alcohol use are also shown to have generally negative impacts on the ocular surface, although evidence is scant in some areas, while caffeine exhibits a protective effect for dry eye, as noted in other reports.
Nutrition
Modifying food consumption habits has potential to lead to better ocular health outcomes⁹. In terms of macronutrients, the strongest evidence of ocular surface benefits favours polyunsaturated fatty acids (omega 3), while for micronutrients, it’s vitamins A, B12, C and D. Dehydration is undesirable, but studies looking at increased water intake have not found it to be protective for dry eye disease. Watch out for excipients, additives and non-nutritional components, such as endocrine-disrupting chemicals that can leach from food containers, as these have documented adverse ocular surface impacts.
Evidence on the impact of intentional food restriction on ocular surface health was sought through a systematic review of 25 studies, mostly focused on Ramadan fasting, but also considering bariatric surgery and anorexia nervosa, but low study quality and a lack of randomised-controlled trials limited the conclusions that could be drawn. Noted, once again, was the good news for coffee-lovers that caffeine was identified as being protective for dry eye disease through increased tear production.
The gut microbiome also plays an important role in regulating low-grade chronic inflammation. Dry eye disease has been linked to marked gut dysbiosis and low microbiome diversity and there’s evidence that pre- and probiotics can improve dry eye signs and symptoms.
This subcommittee report concluded that nutrition and resulting diseases can influence ocular surface inflammation, innervation and microbiome as well as dry eye disease signs and symptoms. More research is required to better understand the impacts and it’s recommended that clinicians carefully review current evidence before providing nutritional advice to patients.
Societal challenges
In evaluating societal impacts on ocular surface health, risk factors for ocular surface diseases were mapped against a societal factors framework that’s been used widely in public health to characterise the relationship between the individual, their health and the environment¹⁰. Taking a stepwise approach that considers an increasingly broader perspective each time, the report focuses initially on non-modifiable biological risk factors such as age, sex and ethnicity as well as genetic risk factors; moves through consideration of individual lifestyle, social and community factors; into living and working conditions; and towards regional and global level impacts where socioeconomic, cultural, political and environmental factors can limit access to healthcare. The report culminates in a discussion of the overarching influences of the digital world and communication technology, acknowledging benefits such as telehealth and access to virtual education, along with downsides such as the negative physical, mental and social impacts of technology.
Through systematic review, Covid-19 infection and pandemic-mitigating measures, such as online schooling and facemask use, are recognised as having increased the frequency and severity of ocular surface disease signs and symptoms. Further acknowledged is the likely continuation of such impacts post-pandemic, prompting the recommendation for a proactive approach to intervention and education.
Conclusion
It’s clear that seemingly unrelated and inconsequential choices patients make on a daily basis can have significant, unanticipated impacts on the ocular surface. Careful attention to patients’ lifestyle choices during history-taking and a willingness to discuss risks and options with patients is warranted in considering ocular surface health more holistically, to help mitigate possible adverse effects and optimise quality of life for patients.
The authors acknowledge the steering committee and all members of the TFOS Lifestyle Workshop for their contributions and are grateful to TFOS executive director Amy Gallant Sullivan for fundraising and to industry sponsors who provided unrestricted funds to support the workshop.
The TFOS Lifestyle Workshop results papers are available here.
References
1. Craig J, Alves M, Wolffsohn J, Downie L, Efron N, Galor A, et al. TFOS Lifestyle Report Introduction: A Lifestyle Epidemic - Ocular Surface Disease. Ocul Surf. 2023;28:304-9.
2. Downie L, Britten-Jones AC, Hogg R, Jalbert I, Li T, Lingham G, et al. TFOS Lifestyle - Evidence quality report: Advancing the evaluation and synthesis of research evidence. Ocul Surf. 2023;28:200-12.
3. Jones L, Efron N, Bandamwar K, Barnett M, Jacobs D, Jalbert I, et al. TFOS Lifestyle: Impact of contact lenses on the ocular surface. Ocul Surf. 2023;29:175-219.
4. Sullivan D, da Costa A, Del Duca E, Doll T, Grupcheva C, Lazreg S, et al. TFOS Lifestyle: Impact of cosmetics on the ocular surface. Ocul Surf. 2023;29:77-130.
5. Wolffsohn J, Lingham G, Downie LE, Huntjens B, Inomata T, Jivraj S, et al. TFOS Lifestyle: Impact of the digital environment on the ocular surface. Ocul Surf. 2023;28:213-52.
6. Gomes J, Azar D, Baudouin C, Bitton E, Chen W, Hafezi F, et al. TFOS Lifestyle: Impact of elective medications and procedures on the ocular surface. Ocul Surf. 2023;29:331-85.
7. Alves M, Asbell P, Dogru M, Giannaccare G, Grau A, Gregory D, et al. TFOS Lifestyle Report: Impact of environmental conditions on the ocular surface. Ocul Surf. 2023;29:1-52.
8. Galor A, Britten-Jones A, Feng Y, Ferrari G, Goldblum D, Gupta P, et al. TFOS Lifestyle: Impact of lifestyle challenges on the ocular surface. Ocul Surf. 2023;28:262-303.
9. Markoulli M, Ahmad S, Arcot J, Arita R, Benitez-Del-Castillo J, Caffery B, et al. TFOS Lifestyle: Impact of nutrition on the ocular surface. Ocul Surf. 2023;29:226-71.
10. Stapleton F, Abad J, Barabino S, Burnett A, Iyer G, Lekhanont K, et al. TFOS lifestyle: Impact of societal challenges on the ocular surface. Ocul Surf. 2023;28:165-99.

Professor Jennifer Craig is chair of the TFOS Lifestyle Workshop and was vice-chair of TFOS DEWS II. She is head of the Ocular Surface Laboratory (OSL) in the Department of Ophthalmology at the University of Auckland.

Dr Kalika Bandamwar served as a member of the TFOS Lifestyle Workshop subcommittee on the impact of contact lenses on the ocular surface and is a post-doctoral research fellow with OSL.