A ‘hot pot’ of ocular insights
More than 150 optometrists attended the Hyundai Marine Sports Centre in Auckland in April for Eye Institute’s autumn seminar. As well as a spectacular sunset, guests were treated to a ‘hot pot’ of ophthalmic CPD and delicious platters.
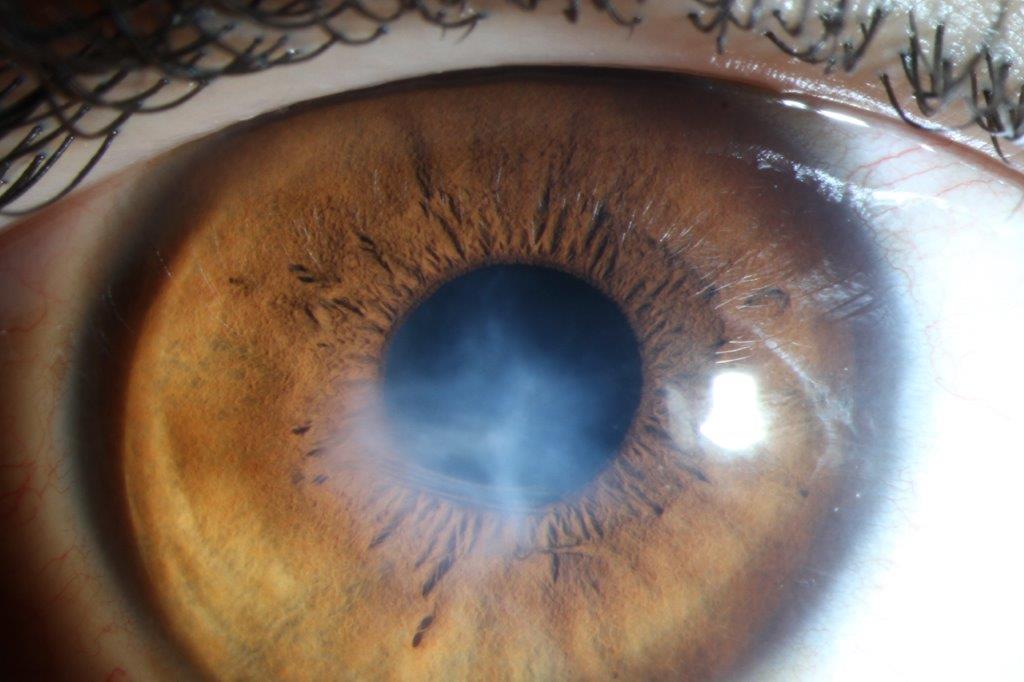
Kicking off proceedings, Dr Adam Watson shared insights into what could happen after cataract surgery. Unlike the usual suspects, such as light sensitivity and gritty or stinging eyes, post-cataract endophthalmitis (1 in 2,000) was a serious side effect requiring urgent referral. Patients typically presented in the first one-to-two days post-surgery or at six weeks. Symptoms included poor vision, aching, painful red eye, a hazy cornea/anterior chamber plus potentially a hypopyon and presence of vitreous cells, requiring immediate treatment to prevent sight loss.
Dr Watson also discussed refracting an extended depth of focus (EDOF) or multifocal lens. With the elongated focus these lenses provide, optometrists need to “push the plus, because if you don’t, the end point is not at the right place,” he said. He recommended to start adding ‘plus’ until blur was reported; add +0.25 more to be certain; only use minus lenses when this first step has been completed; refract astigmatism; check if more plus could be added; and finally, check intermediate and near vision as well as distance before any ‘add’.
Summarising, Dr Watson said successful management of patient concerns required teamwork, understanding and good communication.
Glaucoma diagnosis – clear as mud
Dr Kaliopy Matheos presented glaucoma cases, which she jokingly said were sometimes “as clear as mud”, using the Rubik’s cube as a metaphor for problem solving. With glaucoma, it is important to stick with the algorithm: take a good history, test colour vision, check for relative afferent pupil defect (RAPD) and perform gonioscopy. Findings that required special attention included: patient was younger than 50 years old, of Māori or Polynesian descent, had a marked asymmetry or unilateral optic nerve involvement, unexplained visual acuity loss, colour vision defects and RAPD (in the absence of advanced visual field (VF) defects), VF defects (not corresponding to or out of proportion to optic nerve damage/vertically aligned/altitudinal VF defects), OCT retinal nerve fibre layer (not involving superior and inferior rim or ‘Bow-tie’), optic nerve pallor in excess of cupping, atypical neurological symptoms and normal intraocular pressure (no family history, no history of steroid use, normal angle configuration).
A complete work-up, plus attention to red flags, is key and could be lifesaving as it allows eyecare practitioners to identify glaucoma masqueraders, such as compressive and non-compressive optic neuropathy, Dr Matheos concluded.
Dr Narme Deva shared a series of case studies discussing the clinical manifestation and causes of peripapillary choroidal neovascular membrane (PCNVM) accounting for 10% of all CNVM. While there were multiple aetiologies, a significant proportion (>30%) were idiopathic and a vast majority of patients were asymptomatic until they reached an advanced stage. Treatment was required when PCNVM was vision-threatening and while anti-VEGF was the mainstay treatment, thermal laser and photodynamic therapy were starting to have a larger role, she said.
Dr Kevin Dunne presented on branch retinal artery occlusion (BRAO), central retinal artery occlusion (CRAO) and transient monocular visual loss (TMVL) - medical events he described as the tip of the iceberg, as they could be associated with significant patient morbidity and mortality. A BRAO patient who experiences sudden onset of headache, confusion, numbness/weakness in face, arms or legs and had dizziness or balance issues needs urgent medical attention, he said.
On a lighter note, Dr Graham Reeves tackled the slightly convoluted topic of biomarkers and endpoints in glaucoma. To properly assess the validity of a biomarker, it was all about the outcome, he said. Meanwhile, guiding the audience on a journey through modalities, Dr Peter Hadden highlighted the advantages of different imaging modes for different diagnosis.
Eye Institute will hold its Annual Scientific Conference 2024 on 10 November at the Aotea Centre, Auckland.