Broome with a view
My optometrist wife, Amanda, and I were supposed to have spent July helping out at Lions Outback Vision in Broome. I would give the hardworking ophthalmologists a break and supervise the registrar, while Amanda helped out with some refractions, dispensing and teaching the Western Australian optometry students who rotate through town. I’d also planned to undertake some research. Unfortunately, due to family health issues, we had to postpone our visit. So when the opportunity arose to attend the director of Lions Outback Vision Associate Professor Angus Turner’s post-RANZCO Congress satellite meeting in Broome, it was too good a chance to miss.
The day-and-a-half meeting was held on the famous Cable Beach, where the temperature was in the low 30s. I completed a trio of Kiwi attendees, which included Dunedin house surgeon Dr Waldir de Souza and optometrist Elizabeth Reay. The meeting was entitled ‘Artificial intelligence in eyecare’, with a particular focus on its application to Indigenous peoples.
Shaun Tatipata, an Aboriginal Fred Hollows Foundation manager from Darwin, kicked things off with a welcome, setting the scene before discussing the challenges and opportunities in tackling eyecare in Indigenous populations. He explained Aboriginal Australians have a seven times greater rate of traumatic eye injuries than their non-Indigenous compatriots. In 1980, vision loss was 10 times greater than in other Australians and although this has now decreased to triple the rate, there is clearly still work to be done.
Peter Larsen, who helped establish Specsavers in Australia and is now with Chemist Warehouse, presented his concerns about undiagnosed glaucoma. He discussed how teleophthalmology and clinical communication platform Oculo has transformed the quality of optometry referrals in Australia, and how optometrists are now performing more computerised visual field (VF) tests which will hopefully detect more glaucoma. New technology on the Topcon OCT dashboard will also inform practitioners of the clinical need for a VF test – a positive behaviour change, he said.
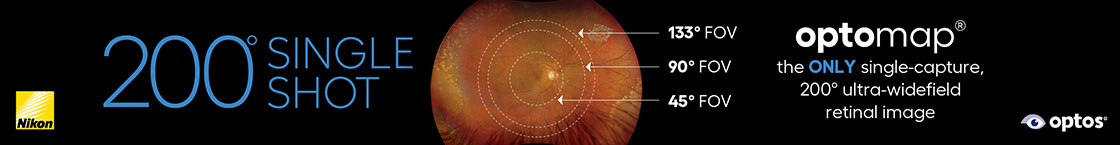
Rory Pilgrim from Google in San Diego talked about automated retinal disease assessment (ARDA), an AI-driven platform developed in 2016. ARDA uses a colour retinal photo to estimate the sex, age, blood pressure, BMI, smoking status and glycosylated haemoglobin (blood sugar) level of the patient. Stunning! Although ARDA has now been launched on the European Optos camera system, Pilgrim explained the demand for such AI use has been bottlenecked by developers not building the products.

Drs Lize Angelo, Rachael Niederer, Nazima Ali and Hannah Ng
The algorithm section
The absolute highlight talk came courtesy of Moorfields’ medical retina consultant and UCL head of artificial medical intelligence Professor Pearse Keane, who discussed assessing whole-body health from an eye image.
In the UK, 10% of NHS outpatient work is ophthalmic, making it the busiest specialty, so he suggested AI could ease this burden. For example, Moorfields receives 7,000 wet age-related macular degeneration (AMD) referrals a year, of which only 800 are ultimately diagnosed as wet AMD. Using the incomparable Moorfields dataset of more than 20 million colour retinal photographs and OCT scans, his team developed an AI algorithm to triage these referrals and improve efficiency five years ago. Although the algorithm works, unfortunately, it will still be some time before it’s incorporated into optometry practice.
Prof Keane also discussed oculomics – how retinal imaging contains a wealth of biological data. For example, the Rotterdam Study described OCT changes in dementia, the AlzEye Study and UK Biobank have also explored dementia, and there has also been published work on retinal changes in Parkinson’s disease and schizophrenia. To foster rapid realisation of these screening pathways, Prof Keane developed the open-source RetFound – a free foundation model for generalisable disease detection. Our Dunedin Study has already published on all these topics and we will be examining them further in April 2024 when the study’s subjects (all aged 52) will return for assessment.
Continuing this theme, CERA deputy director Professor Robyn Guymer described how the volume and morphology of retinal fluid on a macular OCT of a patient with AMD could be evaluated by an AI programme to individualise the frequency of anti-VEGF injections.
The best audience response, however, was received by Dr Karthik Srinivasan from Aravind Eye Hospital, Chennai, India. The hospital is undertaking 2,900 teleconsultations per day from its 105 vision centres. To improve efficiency, they use the Google grading system for diabetic retinopathy, said Dr Srinivasan. Additionally, by employing young women as technicians and photographers in these vision centres, they are preventing them being married off young, educating them, widening their horizons and preventing them being regarded as a burden by their families.
We then broke out into a workshop in a wealthy businessman’s art gallery, which was filled with impressive pieces and set in 14 acres of stunning tropical gardens. Amid these breathtaking surroundings, we pondered how AI might improve the patient pathway in terms of clinical, operational, logistical and research scenarios and how the ‘leaky pipe’ could be patched with new technology or AI.

Dr Graham Wilson and A/Prof Angus Turner
Not only was this satellite meeting free – huge thanks to sponsors: Alcon, Topcon, Heidelberg, Apellis, Roche and The Fred Hollows Foundation - and the Lions Outback Vision team splendid hosts, but being in Broome and watching the sun set over the Indian Ocean made for a memorable conclusion to a wonderful event.
Dr Graham Wilson is a Gisborne-based ophthalmologist, principal investigator for the vision component of the Dunedin Study and an honorary clinical associate professor of ophthalmology with the Department of Paediatrics and Child Health at the University of Otago.