CCLSNZ 2022: Looking back to the future
Fittingly for the Back to the Future theme, delegates and exhibitors took what appeared to be a jump back in time at August’s Cornea and Contact Lens Society (CCLS) conference in Auckland – back to when it was the norm for more than 100 like-minded individuals to congregate, be intellectually stimulated and socialise. Indeed, following a couple of inevitable Covid-related delays, the 2022 conference proceeded successfully, with three international speakers, no less!
Bridging the optometry-ophthalmology divide
Both of this year’s fantastic keynote speakers discussed topics appealing to every member of the audience – an audience unique among ophthalmic conferences, having both optometrists and ophthalmologists in large number. Sydney University ophthalmologist and vision researcher Professor Gerard Sutton, who has clinical and research interests in cataract, corneal and refractive surgery, represented ophthalmology, while Perth-based specialist contact lens and vision rehabilitation practitioner Damon Ezekiel represented optometry.

CCLS speakers Alex Petty, Damon Ezekiel, Prof Gerard Sutton and Dr Richard Hart
Both speakers discussed some of the newer options for correcting presbyopia. Prof Sutton discussed the use of therapeutic agents, which mainly included muscarinic agonists such as pilocarpine to induce miosis and increase depth of field, plus others that reduce the stiffening of the crystalline lens. It appears these latter options are still limited, but it is encouraging to see this area of treatment progressing. It was also interesting to note that multifocal intraocular lenses (IOLs), such as extended-depth-of-focus lenses, are improving and are now a reasonable choice to consider for our patients, particularly since they also come in toric options.
Ezekiel’s presentation on the use of multifocal rigid gas permeable (RGP) lenses was intriguing, especially the importance of lid interaction with translocating bifocals (of course, if the lens does not translocate, it will not work). Prof Sutton also stimulated thought with a fascinating talk on bioengineering corneas. It would appear that artificial corneas are just over the horizon, with all the different corneal cell types now able to be cultured in a laboratory.
Ezekiel’s talk on fenestrated scleral lenses and their use in paediatric cataract cases from as young as four weeks old also generated much discussion. These types of lenses are not used commonly in New Zealand but given the reaction to his talk and the benefits outlined – better handling, less fogging and suction and less intraocular pressure (IOP) effects – there was a great deal of interest in them being introduced and more widely used here.
VR, pterygia or not, and a plethora of research
Dr William Cunningham, ophthalmologist at Auckland City Hospital and Eye Institute, presented fantastically on refractive vitreoretinal (VR) surgery. The art of VR surgery has advanced significantly, alongside the visual expectations of patients, so it was heartening to hear that combined cataract and vitrectomy surgery had highly predictable visual outcomes. I feel much more comfortable reassuring my patients that they are likely to have a good outcome having both operations at the same time. Another interesting takeaway from this talk was the revelation that there is little evidence to support the once widely held notion that bungee jumping or sky diving could cause retinal detachments!
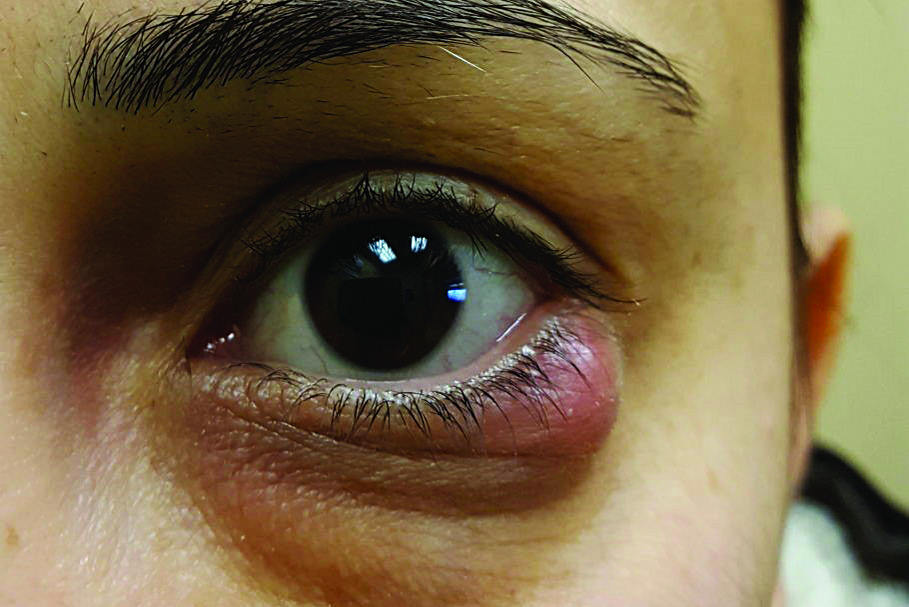
Hospital-based senior optometrist Richard Johnson’s presentation on when a pterygium is not a pterygium highlighted the surprising frequency with which pterygia are in fact neoplasms (benign or malignant). The results of his team’s audit at Greenlane Clinical Centre showed a far greater number of neoplasia than some papers have reported, suggesting that all pterygia should be sent to pathology to determine their composition, as ocular cancers need to be treated as early as possible for the greatest chance of a successful outcome.

Wilson Sue, Radiant’s Yvette Beattie and Leanne Fierro with Dr Lize Angelo
The rapid-fire junior research fellow presentations highlighted some of the interesting work being carried out by our up-and-coming junior doctors, indicating the future of ophthalmology, particularly cornea and anterior segment, is in good hands. We await the results of Dr Lize Angelo’s PhD investigation into keratoconus referral patterns in New Zealand with great interest, as it should aid enormously with understanding how we can ensure appropriate and timely keratoconus referrals.
Dr Angelo also spoke about the repeatability and comparability of different corneal topography and tomography devices. It was rather interesting to note that the Medmont E300 – probably the most common topographer among Kiwi optometrists – is highly repeatable in keratoconus. However, its inability to measure corneal thickness does severely limit its usefulness in monitoring keratoconus and triaging referrals for crosslinking. On a similar theme, Dr Himanshu Wadhwa demonstrated that the Oculus Pentacam AXL, a corneal tomographer with integrated axial-length measurement, is less repeatable when measuring pachymetry and keratometry in advanced keratoconus, thus clinicians should have a higher threshold for change in these parameters when assessing disease progression in advanced ectasia.
Continuing this research focus, Dr Joevy Lim presented on the outcomes of plaque brachytherapy for choroidal melanoma, indicating it could be a useful management strategy for small- and medium-sized tumours but can have devastating effects on patients’ vision. Dr James Lewis, Auckland University's newest research fellow, focused on the different ways of improving pain, post de-epithelialising procedures (such as PRK and crosslinking). He showed that simple options such as using a bandage contact lens soaked in the non-steroidal anti-inflammatory drug Acular (ketorolac trometamol) or chilling the riboflavin pre-crosslinking can be surprisingly effective at reducing pain.

Dian Zhuang and Aimee Aitken with Drs Himanshu Wadhwa, Aki Gokul and Joevy Lim at Friday dress up gala dinner
Amniotic membranes, artificial irises, CXL and some thanks
Also kindly making the trip across the Tasman to join us and share their significant knowledge of contact lenses and anterior segment eyecare was CCLS 2022’s third international speaker, Margaret Lam, CCLS Australia’s former president and now current president of Optometry Australia. She provided a highly insightful and practical presentation on the use of amniotic membranes, discussing several cases, including severe dry eye and post-chemical injuries, where the results were simply outstanding. Though her talk and trip were sponsored by AmnioTek amniotic membrane graft supplier Medix21, she prefaced it by saying she was so enamoured of the product’s ability to treat tough cases, she’d have happily flown over and given the talk without any sponsorship!

CooperVision’s Dr Joe Tanner with fellow speakers Margaret
Lam, Debra So and Dr Mo Ziaei
Now based in New Plymouth, former Auckland-based paediatric optometrist and clinical researcher Dr Samantha Simkin discussed the use of soft contact lenses with an artificial iris for albinism, which produces excellent outcomes in certain cases. Her talk on the normative refractive error and axial length values was also superb, with an excellent take-home message: “Children should be low hyperopes, and keep myopes under 26mm if at all possible!”
Auckland-based consultant ophthalmologists Drs Rasha Altaie and Mo Ziaei provided updates on the use of AI in keratoconus and crosslinking (CXL), respectively. AI still has some way to go to accurately diagnose keratoconus but is likely to be an effective tool for keratoconus screening in the not-too-distant future. As for treating keratoconus, accelerated crosslinking is highly effective and efficient, particularly when patients are treated early enough, so all patients under the age of 18 should be referred at diagnosis, with no evidence of progression needed, said Dr Ziaei. This view was supported by others in the audience and presenter Debra So, allied health clinical team leader in ophthalmology in Counties Manukau. She discussed the success of the Counties Manukau optometrist-led keratoconus clinic, established in direct response to the worrying number of overdue appointments. This new model of care allowed for increased capacity in consultant clinics and earlier disease progression detection and CXL treatment, clearly demonstrating how a clinic such as this can be run very successfully by optometrists with ophthalmology oversight.
This year’s conference was wrapped up by Auckland University’s head of ophthalmology and corneal specialist Professor Charles McGhee, who elegantly summarised the developments in eyecare and research in Aotearoa over the past 20 years. His presentation highlighted the remarkable leaps and bounds made in New Zealand – we truly do punch above our weight in many areas of research and disease management.
And finally, on behalf of the CCLS council, I’d like to thank the sponsors who made the conference possible. This year’s trade show was exceptional, with plenty of new technology on display, including the latest and greatest in OCT and corneal tomography. Thank you to our platinum sponsors, Bausch + Lomb and the Ophthalmic Instrument Company (OIC); our premium sponsors, Alcon, Coopervision, and Optimed; our partner sponsors, Designs for Vision, Device Technologies, the Corneal Lens Corporation, Johnson & Johnson Vision Care, and Medix 21; and for the sponsor donation from Precision Contact Lenses.
Following the success of this year’s conference, I’m greatly looking forward to our next one-day conference in 2023. See you there!
CCLS councillor Dr Akilesh Gokul is a clinician-scientist, an optometrist specialising in contact lenses at Mortimer Hirst Optometrists and a senior lecturer in Auckland University’s ophthalmology department. He also works with the Auckland District of Te Whatu Ora’s crosslinking service. His main clinical and research interests include keratoconus, contact lenses, crosslinking and inequity in healthcare.