Championing dry eye research and collaboration at home and afar
If Covid-19 has taught us anything, it’s that we should take nothing for granted and we should seize opportunities to spend time with family and friends, to have the courage to take on a new challenge, or at least to challenge the status quo.
Conferences and meetings are now often offered in a convenient hybrid format, yet it seems, for the majority, this hasn’t dampened the desire to meet face-to-face. As I prepare to set off for my third international conference since the country’s borders re-opened, I’m reassured by the reports of others that my sense of trepidation is far from unique but, like others, it doesn’t outweigh my excitement at finally being able to re-connect with peers overseas.
The recent border openings will undoubtedly herald an influx of international migrants and visitors to New Zealand in coming months and, for us here at the Ocular Surface Laboratory (OSL) at Waipapa Taumata Rau | The University of Auckland, it’s a chance for cross-pollination of research, to exchange knowledge and to gain new skills. We’re pleased to welcome our newest OSL postdoc, Dr Kalika Bandamwar, who has waited patiently for two years to join our research team. Sadly we farewell Dr Alex Müntz, who’s been a highly valued OSL team member for more than four years. While we’ll miss him terribly, we’re delighted he will retain a strong, albeit remote, connection with our team to further existing collaborative projects and jointly supervise postgraduate research. We continue to value other international collaborations within our broader research plan, as highlighted in the various articles throughout this issue, with many articles penned by returning authors and some new, from as far afield as Glasgow and Birmingham in the UK to Sydney and Melbourne in Australia and Miami in the US.
In Aotearoa, the OSL team has been working harder than ever since the Covid-related restrictions of late 2021 that denied staff and students access to the university for nearly four months. Trials set for last year were mostly delayed until this year, so we look forward to sharing their outcomes in future issues of NZ Optics. As an overview, however, our latest research projects continue to explore different facets of dry eye disease (DED) – its epidemiology, pathophysiology, diagnosis and management. We continue to work on better understanding the natural history and risk factors for DED via an ongoing longitudinal study of optometry students, led by Bhavna Patel, with BOptom honours students George Zhou and Jiwoon Kim, a study focusing on the ocular surface of Māori, with summer student Saia Manase. Partnership with Māori has supported other research that ultimately seeks to address inequities in ocular health outcomes for Māori. Isaac Samuels, a current BMedSci honours student describes some of the findings of a recent HRC summer studentship project completed together with BNurs (Māori) student Julie Pirere, which aimed to discover Māori participants’ thoughts on eye health and perceived barriers to obtaining optimal care.
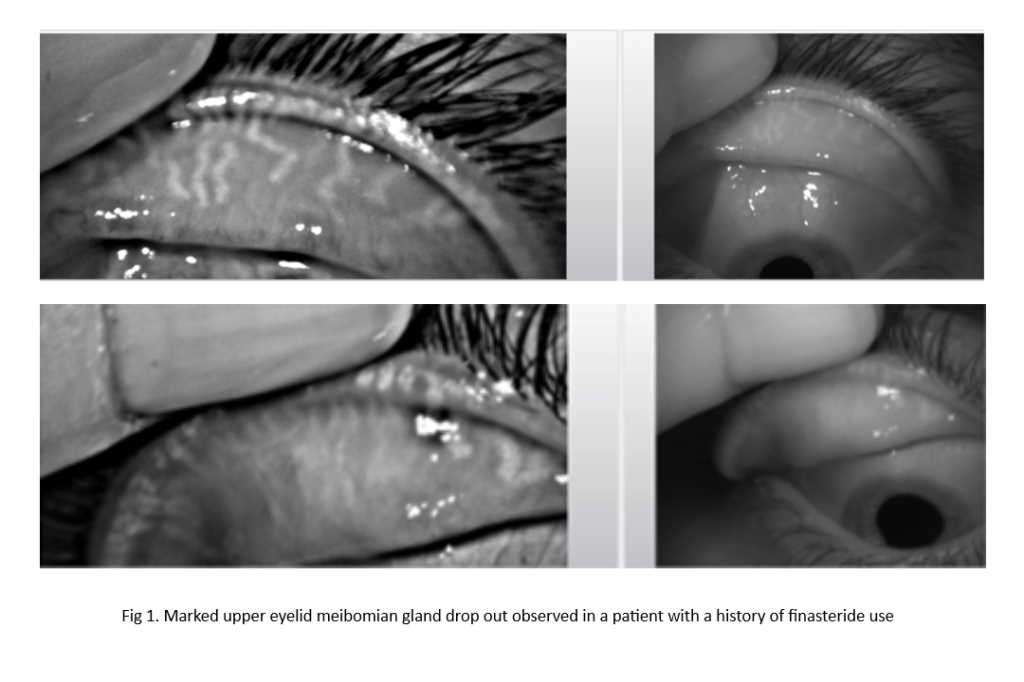
At the OSL, we continue to challenge our ability to accurately diagnose, classify and monitor DED for both research and patient care. Recent diagnostic accuracy studies have focused on assessing the performance of newer clinical devices such as E-Swin’s Tearcheck, as well as the Topcon MYAH as part of a multicentre international study. Dr Alex Müntz has been exploring possible new eyelid margin markers for meibomian gland dysfunction (MGD); Catherine Shon submitted her Masters’ thesis evaluating clinical indices of ocular surface inflammation against laboratory markers; and Dian Zhuang continued her PhD studies evaluating inflammasomes in ocular surface disease and their potential as a target for future therapy. Dian and Catherine, working closely with 2021 BOptom honours student and summer student Carmen Liu, share the outcomes of their study comparing tear collection methods on.
Through carefully designed, randomised controlled clinical trials that seek to reduce the risk of bias, the OSL team has also been exploring the efficacy of some exciting new dry eye therapies. This includes the evaluation of Azura Ophthalmic’s keratolytic eye preparation AZR-MD-001. Led locally by team member Eva Pheng (BOptom Hons), OSL is one of several trial sites across New Zealand, Australia and Canada. Recruitment for the six-month trial is now closed and we eagerly await the study outcomes in coming months, which could ultimately see the commercialisation of the first dedicated pharmacotherapy for MGD. We also have industry-supported, investigator-initiated trials underway involving in-office devices such as the iLux thermal pulsation device (Alcon), led by clinical researcher and optometrist Catherine Shon, and the Rexon-Eye device (Quantum Molecular Resonance; Resono Ophthalmic), led by Ryan Mahmoud from his optometry practice (nVision Eyecare, Albany) and Dr Alex Müntz through the university. Now in the final stages of recruitment, both trials are expected to be completed towards the end of the year.
As well as reviewing devices, we continue to have an interest in artificial tear supplements with a BOptom Honours project currently underway, led by Kevin Chen and Ju Ee Wong, comparing layered aqueous and lipid drops to a combined aqueous-lipid formulation. We’re also excited to be working with TRG Natural Pharmaceuticals and natural health physician Dr Emma Sandford, on a brand new investigator-initiated randomised controlled trial to explore the benefits of a proprietary castor oil formulation for periocular application in blepharitis.
A better understanding of dry eye disease will serve to improve quality of life for affected individuals. The OSL team is privileged to continue our work in this field, while being in awe of the amount of work going on globally. We’re thrilled that the latest Tear Film and Ocular Surface Society (TFOS) workshop, ‘A Lifestyle Epidemic: Ocular Surface Disease’, is nearing completion and due for submission for publication in a few months’ time. I’ve been honoured to chair this global initiative, working alongside Dr Monica Alves (vice-chair), David Sullivan (organiser) and 11 fantastic subcommittee chairs and together with more than 150 expert workshop members from around the world. This global consensus report focuses of the multitude of factors we’re exposed to within our everyday lives and highlights how the choices we make can affect our ocular surface. Its outcomes will undoubtedly provide a wealth of information for clinicians around the world in helping to manage ocular surface disease in their patients.

Professor Jennifer Craig heads up the Ocular Surface Laboratory at the University of Auckland’s Department of Ophthalmology, was vice chair of TFOS DEWS II and is currently chair of the next TFOS’ workshop, ‘A Lifestyle Epidemic: Ocular Surface Disease’.