Dry eye and cosmetics: a clinical experience
It started with dirty lashes! A keratoconic patient had tried something new and while they looked fabulous, on closer inspection, the bases of her lashes were caked in debris and collarettes, which got me thinking there must be a better way for our patients to look their best without negatively impacting their eyes.
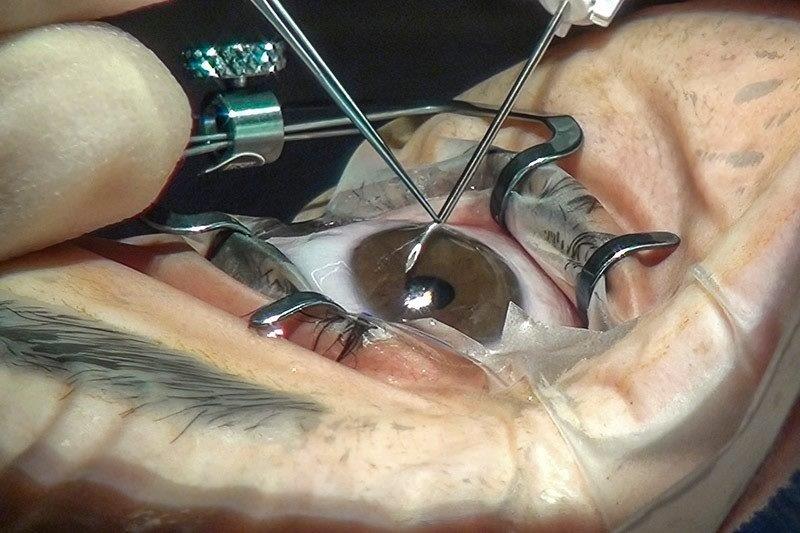
We’re seeing more patients with dry eyes, contact lens intolerance and/or makeup intolerance. We probably all have daily, highly magnified examples of poorly placed or voluminous makeup application. Behind a slit lamp, it’s not so pretty (Fig 1). Beauty will almost always win and I can understand that. Makeup helps with self-confidence and as someone who also looks (more) tired without mascara, I knew it wasn’t going to be as simple as telling my patient to stop wearing makeup. So I began wondering what advice I could give them.
After a fair bit of self-learning and discussion on this issue with international colleagues over the past few years, I have now made cosmetic discussions a routine part of my patient management. The current knowledge, and gaps in our knowledge, have been solidified with the TFOS Lifestyle: Impact of cosmetics on the ocular surface report1.
As well as asking patients about their habits, for several years I’ve been giving my dry eye and contact lens-wearing patients a self-created handout on healthy makeup habits, with both general advice and a range of brand recommendations. In 2022, this evolved into stocking the ‘Eyes Are The Story’ makeup range* which promotes ‘a vision of beauty without compromise’, formulated to be kinder to the ocular surface than many mainstream products whose ingredients have been identified through in vitro studies to present a risk to the health of the ocular surface.
While my goal is ultimately to benefit my patients in general, there are some specific cases which have left an impression.
Case studies
SB is a 34-year-old patient with rosacea and frequent styes who, as a professional musician, feels the need to wear makeup. While managing her underlying meibomian gland dysfunction, the discussion around makeup came to a head one day. She’d been making excellent progress with her clinical signs and symptom scores when she wore “old” mascara for a music video shoot, resulting in one eye flaring up within a day with lid inflammation and a new stye. While she admits to not being the best at makeup removal, we’ve now got her onto both better lid hygiene habits and switched her to the new makeup range with good results.
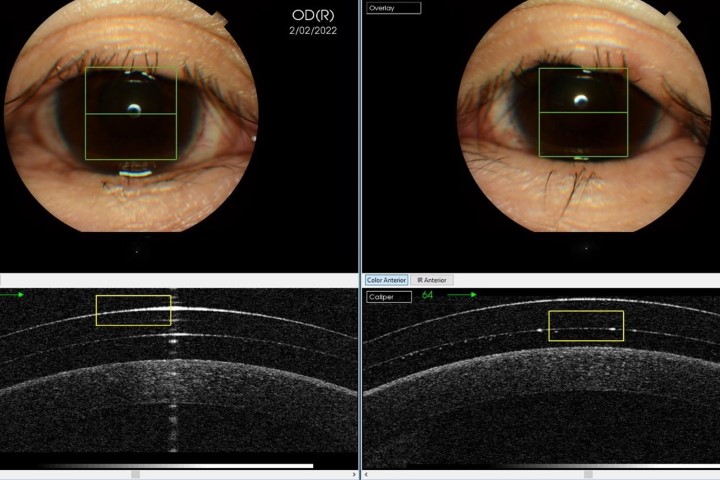
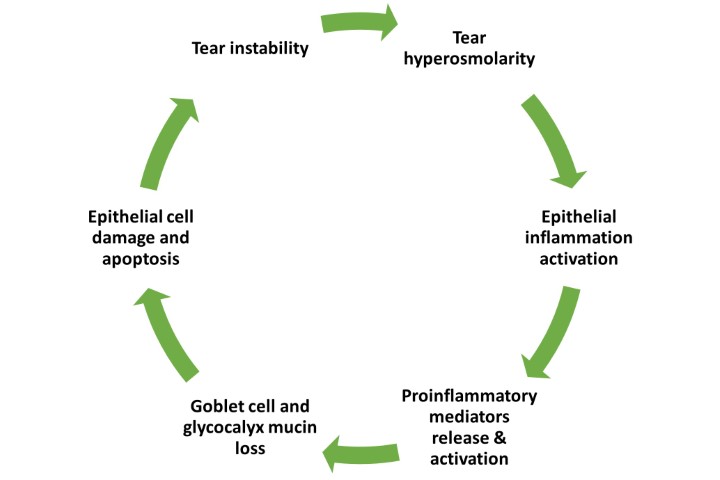
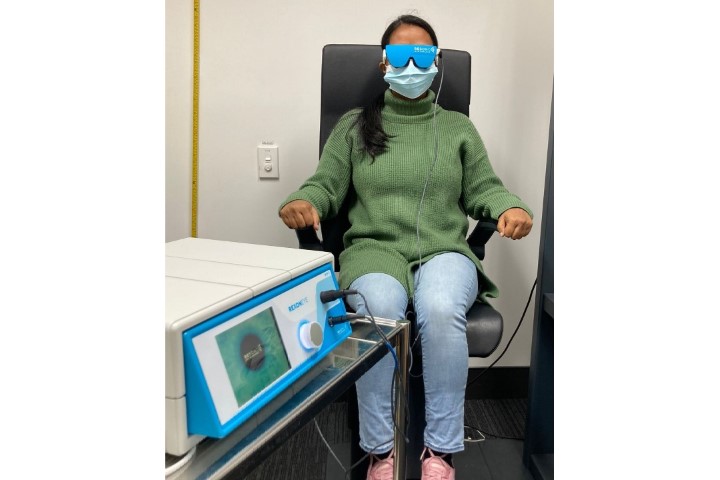
SM is a 58-year-old patient referred to me from her regular optometrist for management of her chronic meibomian gland dysfunction and recurrent styes (Fig 2). She was both desperate to avoid styes and to get back to wearing makeup comfortably. After a period of four months with a course of intense pulsed light (IPL) therapy and therapeutic expression in practice, as well as home management with warm compresses, omega-3 supplements, Optimel antibacterial manuka eye drops, a course of oral antibiotics and a switch to the new makeup brand, we’re at a point where we have comfortably improved the baseline MGD and have her back to looking and feeling her best self.
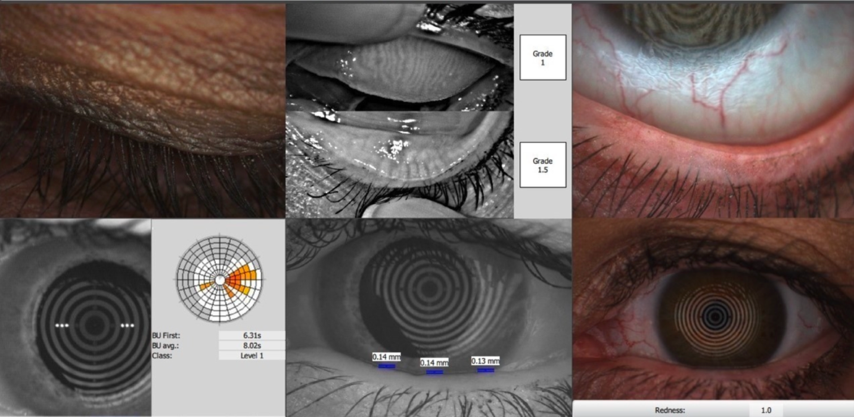
Fig 2. Assessing the patient's MGD
Returning to my keratoconic patient, the conversation centred around cleaning her lash extensions with a hypochlorous spray, as she wished to keep the extensions. Simple changes, however, such as reminding patients to remove their makeup thoroughly each day, can make a big difference. Good eyelid hygiene habits and safer makeup use is a conversation we can all start having with our makeup-wearing patients. Like many things, the more you do it, the easier it gets. We don’t need to tell patients they can’t wear makeup, but we can tell them there’s a safer way to be doing it. As with most aspects of clinical optometry, photographs help with patient education, as do written resources to support your conversations. It’s simple to make your own handout or point patients in the direction of good online information or, if you’re a Cornea and Contact Lens Society (CCLS) member, make use of the CCLS Cosmetic Considerations handout.
*Disclaimer: The Eyes Are The Story makeup range was founded by Amy Gallant Sullivan, executive director of TFOS, which she co-founded with her father, Associate Professor David Sullivan
Reference
1. Sullivan D, da Costa A, Del Duca E, et al. TFOS Lifestyle: Impact of cosmetics on the ocular surface. Ocul Surf 2023; 29: 77-130.

Adele Jefferies is an optometrist working in independent practice in Auckland with special interests in dry eye and ocular surface disease, contact lenses and therapeutics. She is the national clinical manager for Matthews Eyecare and the current president of CCLS (NZ).