ESA: Warming up winter with CPD pearls
Warmed by fairy lights and a strong turnout, Eye Surgery Associates’ mid-winter dinner symposium at the Tamaki Yacht Club in Auckland was packed full of eyecare pearls for attending optometrists.
Keynote speaker Associate Professor Stuti Misra was introduced by Dr Monika Pradhan who outlined her many achievements from Fullbright Scholar to the Asia-Pacific Academy of Ophthalmology Achievement Award in 2017 and being made an American Academy of Optometry diplomate in 2022 for her work on the ocular surface. A/Prof Misra has also secured more than $3 million in research grants for the University of Auckland and published over 50 peer-reviewed papers. Lesser known were her roles as a board director for Fertility NZ, her volunteer work with the Shakti women’s refuge and her love of Bollywood and traditional Indian dancing, which included performing at last year’s Diwali Festival, and being an ardent Kiwi sports fan, said Dr Pradhan.

Robyn Stirling, Vicky Wang, Dr Monika Pradhan and Jas Walia
Issues with fluctuating female hormones
A/Prof Misra was tasked with covering two topics at the symposium: ‘Female hormones, menopause and the ocular surface’; and ‘Systemic diseases: a story by corneal subbasal nerves’.

Kavin Natali, Khyati Jindal and Arshad Hoosen
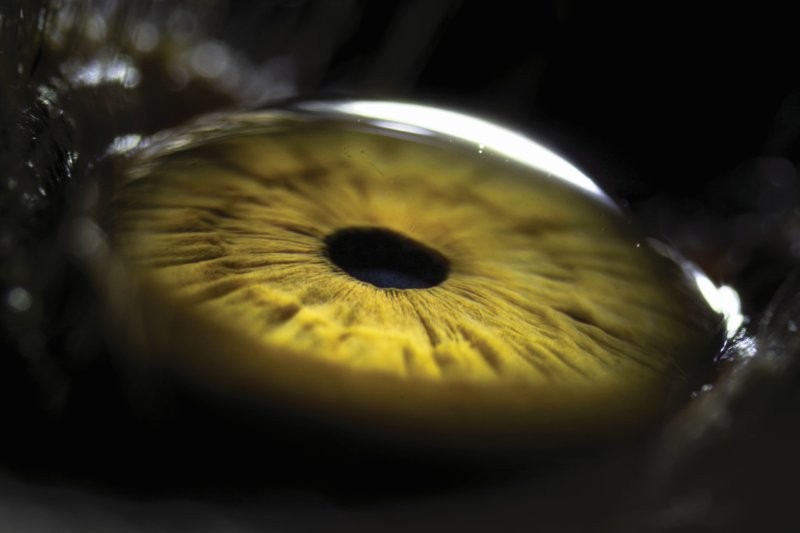
Setting the tone of what was to come, attendees were put through their CPD paces via phone quiz questions as A/Prof Misra discussed how the fluctuation of female hormones through the menstrual cycle, perimenopause and menopause can significantly affect the ocular surface. A low level or absence of progesterone in the lacrimal gland, for example, leads to inflammatory changes, resulting in conjunctival congestion or meibomian gland dysfunction (MGD). These hormonal changes can be exacerbated by lifestyle and environmental factors, she said, such as exercise which can improve tear quantity during ovulation.

Kathryn Sands, John McLennan, Dr Marcy Tong and Sephy Cheng
Menopause increases dry eye disease (DED) symptoms, said A/Prof Misra, including poor tear stability, MGD and poor tear-film secretion. Though there’s limited research on the effects of hormone replacement therapy there is some evidence to suggest it can improve DED symptoms, especially in the under-50s. Other treatments include testosterone eye drops or creams on the eyelids, though using transdermal oestrogen tends to worsen DED symptoms, she said.
Electrophysiology and a closer look at IOP
Dr Tracey Wong provided a practical talk about using different electrophysiology tests for diagnosing visual problems and monitoring and assessing their severity. Visual electrophysiology measures the small electrical signals the retina passes along the optic nerve to the brain which allow people to ‘see’, she said. “Different tests help define location and level of dysfunction.”

Sushmita Chinchankar, Kyla Kubba and Rebecca Kassir
The main test is the electroretinogram (ERG), which measures the electrical activity of the retina in response to light to identify retinal dystrophies. Other tests include visual evoked potential (VEP), which assesses the visual pathway, especially in the optic nerve; electro-oculogram (EOG), which measures retinal pigment epithelium function; multifocal ERG (mfERG), to identify focal retinal pathology; and pattern ERG (pERG) to differentiate macular and optic nerve pathology.

Sandhya Mathew, Priyal Bhoola and Kenny Wu
Dr Hussain Patel then introduced the audience to Swiss physician Ernst Sidler-Huguenin, who was the first to identify intraocular pressure (IOP) variations over a 24-hour period in 1898. Despite this, it’s only recently that the significance of these fluctuations has begun to change the way we think about IOP in glaucoma management. Lowering IOP works, but IOP changes from second to second, day to day and week to month, so the probability that a single pre-treatment IOP test is likely to be at its highest point that day is only about 20%, so it’s probably not that useful, he said.

Maryanne Dransfield with Drs Hussain Patel and Yi Wei Goh
As well as circadian fluctuations, IOP also changes with body posture, blood pressure and other physiological changes in the body, and even varies according to the measuring device you use, said Dr Hussain. “The only constant about IOP is that it is constantly changing.” The future is wearable technology, though currently there’s no clinically available wearable-IOP device that continuously measures IOP over time, is safe, practical and reliable and affordable, but progress is being made, he said. Potential devices include Sensimed’s Triggerfish contact lens monitoring system; the implanted Eyemate sensor, which transmits IOP wirelessly from a handheld reader to the patient’s database; and Injectsense’s ultra-miniature implantable sensor. Until these come to market, however, practitioners should use the tools available, said Dr Hussain, including the water-drinking test, day phasing, the iCare self-tonometer for home testing and booking multiple clinic visits at different times and different days to get a more accurate idea of a patient’s real IOP.
Dealing with dislocated lenses and pterygia
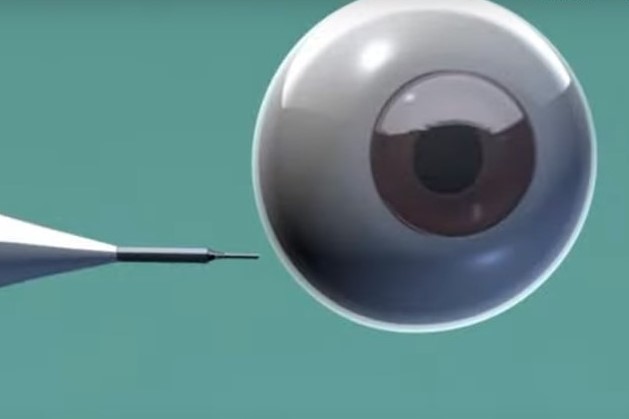
Lens subluxation or dislocation is primarily caused by trauma or complicated cataract surgery, said Dr Pradhan, as well as a host of ocular conditions, including aniridia, congenital glaucoma, high myopia, intraocular tumour and syphilis, or systemic conditions, such as Marfan, Ehlers-Danlos and Sturge-Weber syndrome or homocystinuria. Medical treatments include refractive correction, drops or laser iridotomy for IOP fluctuations and further systemic investigations. Surgical treatments include lensectomy with anterior vitrectomy or posterior pars plana vitrectomy and phacoemulsification using a sutured capsular tension ring, she said, adding treatment will vary depending on the patient’s age and degree of subluxation.
One new treatment is the Carlevale IOL, the first IOL designed specifically for scleral fixation. Suspended behind the iris, it does not tilt or decentre and it’s foldable, so it can be inserted through a small incision, said Dr Pradhan. “I’m very excited about this new lens… it almost looks like a normal IOL in the eye.”

Hue and Michael Bullen with Anna Sue (centre)
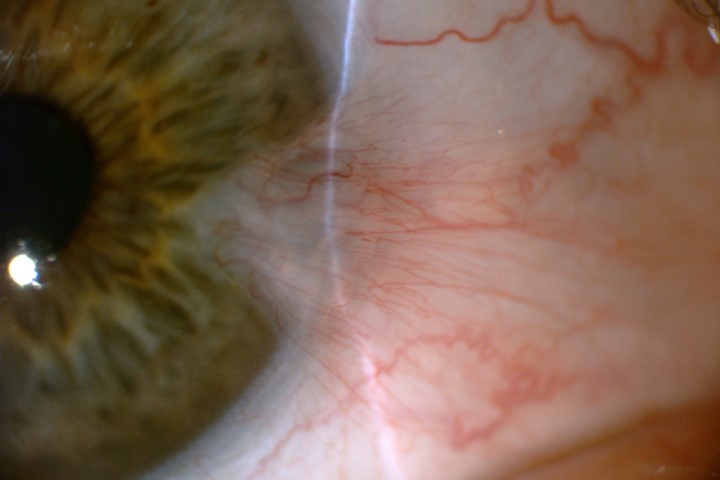
With summer looming, Dr Yi Wei Goh tackled pterygia. Pathogenesis includes UVB light, human papillomavirus and abnormal cell proliferation. Other risk factors include age, male gender, dry eyes, darker skin and hair colour and irritants, such as wind, dust and chronic infection. Referral for surgery is recommended if the pterygium affects the patient’s vision, has an atypical appearance, the patient can feel it or has cosmetic concerns, if it restricts eye movement or to improve contact lens fitting. Conjunctival autografting is the most common surgical treatment, she said, with topical antibiotics and steroids post-surgery. It can be very painful for a few days after surgery, said Dr Goh, and the patient may also experience blurry vision, light sensitivity, watery and red eyes and, less commonly, bleeding or scarring. To prevent pterygia and their recurrence, patients should be encouraged to wear hats and sunglasses, she said.