Eye Donation: factors affecting donation rates in Aotearoa New Zealand
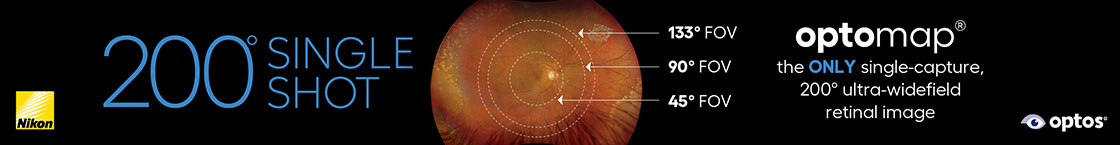
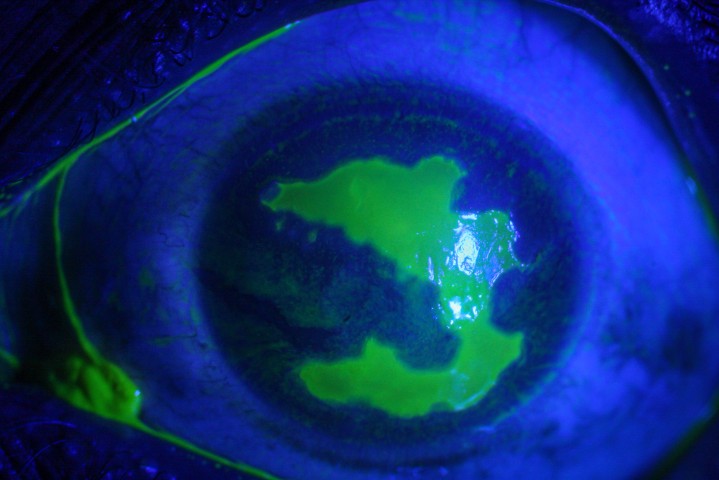
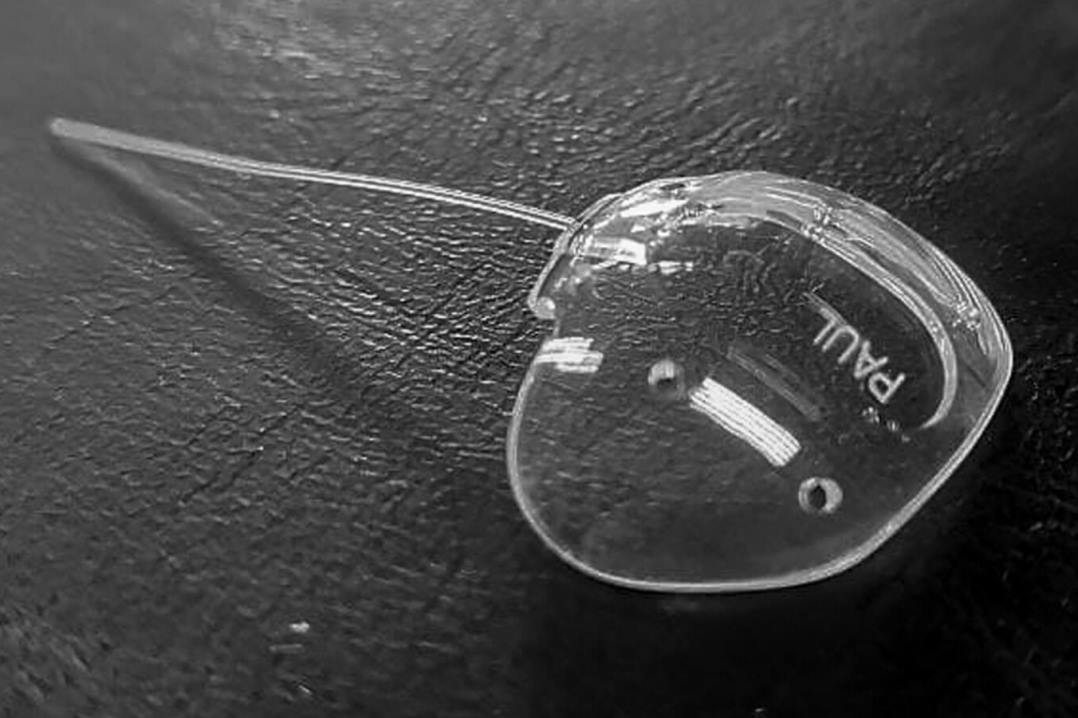
Every year in Aotearoa New Zealand several hundred patients require a corneal transplant. This may be because their cornea is scarred, cloudy or too thin to allow good vision. While we await the invention of the fully fledged laboratory-grown cornea, our principal option to treat these patients is using corneal tissue from a deceased donor for keratoplasty. This can include a number of different surgical procedures that encompass contemporary corneal transplantation, including penetrating keratoplasty (PK), deep anterior lamellar keratoplasty (DALK), Descemet stripping (automated) endothelial keratoplasty (DS(A)EK) and Descemet membrane endothelial keratoplasty (DMEK). All of these procedures require the use of corneal tissue from deceased donors, obtained and processed by the New Zealand National Eye Bank (NZNEB).
Eye tissue donation is very different from organ donation. To be eligible to donate large solid organs, such as kidneys or livers, there are very strict criteria that must be met. Donors are usually defined as a donor after brain death or circulatory death. In both circumstances organs must be removed extremely quickly for them to remain viable. However, this is not the case for eye tissue. Eye tissue may be retrieved and placed in storage up to 48 hours after death, thus the number of eligible eye donors far exceeds the number of eligible solid organ donors in Aotearoa and elsewhere.
The decrease in eye donation rates
Over the last decade, however, the rate of eye donations within New Zealand has been decreasing, while the number of corneal transplants performed has continued to increase. Meeting the recipient demand is only possible due to the significant quantities of corneal tissue imported from Australian Eye Banks (43% in 2023). The scale of the waitlist for corneal transplantation is currently not known, yet we believe the majority of recipients receive their corneal transplant in less than one year.
Importantly, over the past decade, the vast majority (81.4%) of eye donors have died in a hospital setting. By contrast, previously, many eye donations were referred through the coroner when patients required post-mortem autopsies; however, the frequency of these post-mortems has declined substantially recently and there is no longer a dedicated referral coordinator for this pathway. Consequently, in Aotearoa most of our corneal tissue is currently referred through Organ Donation New Zealand and therefore comes from intensive care units (ICU) and critical care departments (DCCM).
Gender, age and ethnic disparities
After performing a statistical analysis on the demographics of eye donation in New Zealand over the past decade (January 2013 to December 2022), several trends emerged. Female gender was associated with a decreased likelihood of eye donation on multivariate analysis. This goes against what is traditionally reported in the scientific literature. Typically, women are more likely to donate their organs than men, which has been attributed to vague notions surrounding increased generosity and empathy of the female temperament. The lower rates of female donation found in our study may be more attributable to the ‘next of kin’ consent, rather than a true reflection of the individual’s intention to donate.
Several studies have analysed the discrepancy between an individual’s intentions to donate their organs and those who actually donate their organs. For example, women are often overrepresented on organ donation registries but can be underrepresented in terms of actual donation rates. Indeed, it has been shown that a male relative is more likely to decline in favour of preserving ‘dignity’ than a female relative, whereas women are more likely to agree to donation on behalf of deceased men.
It was also observed that, over the last decade, eye donation decreased with increasing age. This is another interesting finding that goes against established literature that elderly people tend to be more compassionate and are more likely to want to donate their organs. A possible explanation may be that public knowledge about eye donation is poor, even among health professionals1-4. Indeed, a survey of 371 Australian patients found that 44% thought eye donation could only occur if a patient was declared ‘brain dead’4. In hospice settings, with older, more co-morbid patients, some nurses report feeling uncomfortable bringing up the topic of eye donation, because they are unsure of the suitability of these patients for donation5. These factors may contribute to the lower rates of donation found with increasing age, together with the lack of donation pathways in New Zealand hospices.
Eye donation is not currently part of the palliative care pathway, in contrast to other countries, such as Canada and the UK. Internationally, intention to donate and actual donation rates do appear to be misaligned, with elderly people more likely to be willing to donate when questioned, but less likely to actually donate based on NZNEB data4-7. It suggests there are systemic barriers to eye donation in the elderly that may include inadequate health literacy, dying in the community and poor communication among family members about individual preferences.
Several ethnic disparities were also found through the multivariate analysis of our data. New Zealand Europeans and Asians are more likely to donate their corneas than Māori and Pasifika individuals. The reasons for these differences are unknown and likely complex and related to inequitable access to healthcare as a whole. Further study is required to understand the mechanisms at play.
Decline in donors not simply Covid-related
The decline in eye donation rates identified over the past three years in the Covid era is ubiquitous, globally. Several international eye banks have reported a sharp decline in donation numbers during and immediately after the pandemic9,10. This is easily attributed to poor access to healthcare services, fear of Covid transmission through graft tissue and general breakdown of systems during the global pandemic.

Fig 1. Source of corneal donors in the last decade
It is more challenging to evaluate the less marked, but steady decline in eye donation rates in Aotearoa leading up to the pandemic, which is a consequence of having few resources for facilitating donation conversations. There are also significantly fewer coroner cases now compared with the previous decade, due to a gradual policy change11. Over the last decade, only 14.4% of eye donations came from this pathway in New Zealand.
By law in Aotearoa, the consent to donate any organ or tissue, including corneas, must be given by the next of kin. Individuals may express their preference for donation on their driver’s licence but this is not legally binding (as it is in some states of America, for example)¹². Overseas studies have shown that in cases where the topic of organ donation has never been discussed with an individual, family members are far more likely to decline.
There is also no formal donor registry in this country for corneas or otherwise and, importantly, there are currently no donor programmes in Aotearoa which systematically offer donation for patients outside the ICU, so the next of kin are not routinely offered the opportunity for donation. Thus, in summary, the biggest problem is a lack of suitable donor pathways in New Zealand.
A new donation pathway?
Fortunately, the NZNEB is making significant and exciting changes to offer eye donation to a wider range of patients in New Zealand. A new tissue donation pathway is being created in Auckland through a partnership between the NZNEB and the NZ Blood Service’s Organ Donation New Zealand (ODNZ) service to offer the opportunity for eye donation outside the ICU. This will involve a new specialist nurse coordinator to facilitate the eye donation process, which should lead to significantly increased donation rates.
This article was based on a recent paper published in Cornea.
References
- Chumkasian W, Fernandez R, Petsoglou C, et al. Prevalence and predictors of knowledge and attitudes toward eye donation among the general population: a systematic review. Cornea. 2023;42(4):520-528.
- Mack R, Mason P, Mathers W. Obstacles to donor eye procurement and their solutions at the University of Iowa. Cornea. 1995;3(14):249-252.
- Abuksis G, Orenstein S, Hershko A, et al. Cornea recipients: are their opinions and attitudes toward organ donation different from those of the general population? Transplant Proc. 2004;36(5):1249-1252.
- Essman C, Lebovitz D. Donation education for medical students: enhancing the link between physicians and procurement professionals. Prog Transplant. 2005;15(2):124-128.
- Lawlor M, Kerridge I, Ankeny R, Dobbins T, Billson F. Specific unwillingness to donate eyes: the impact of disfigurement, knowledge and procurement on corneal donation. Am J Transplant. 2010;10(3):657-663.
- Williams A, Muir K. Awareness and attitudes toward corneal donation: challenges and opportunities. Clin Ophthalmol. 2018;Volume 12:1049-1059.
- Liu Y, Zhang Y, Liu Y, et al. Demographic characteristics of voluntary donors registered in Beijing Tongren Hospital Eye Bank of China: a retrospective study from 2007 to 2016. Transplant Proc. 2017;49(8):1712-1718.
- Ranjan A, Das S, Sahu S. Donor and tissue profile of a community eye bank in Eastern India. Indian J Ophthalmol. 2014;62(9):935-937.
- Aiello F, Gallo Afflitto G, Pocobelli G, Ponzin D, Nucci C. Effect of Covid-19 on eye banks and corneal transplantations: current perspectives. Clin Ophthalmol Auckl NZ. 2022;16:4345-4354.
- Aiello F, Genzano Besso F, Pocobelli G, et al. Corneal transplant during Covid-19 pandemic: the Italian Eye Bank national report. Cell Tissue Bank. 2021;22(4):697-702.
- Ang M, Moriyama A, Colby K, et al. Corneal transplantation in the aftermath of the Covid-19 pandemic: an international perspective. Br J Ophthalmol. Published online July 30, 2020:bjophthalmol-2020-317013.
- Douglas T, Douglas N. Absence of significant dissent should be sufficient for deceased donor organ procurement in New Zealand. Aust N Z J Public Health. 2009;33(5):449-454.

Dr Natalie Allen is a junior registrar and PhD candidate working in the University of Auckland’s Department of Ophthalmology.

Eye-banking specialist Nigel Brookes is a senior technical officer with the NZNEB, which was established in 1991 and is based within the University of Auckland’s Department of Ophthalmology.

Eye-banking specialist Maureen Watson is a donor coordinator with the NZNEB.

Eye-banking specialist Helen Twohill is a donor coordinator with the NZNEB.