Finding relief with scleral lenses
This article discusses a dry eye patient with persistent corneal staining who was successfully managed at my private practice using scleral contact lenses.
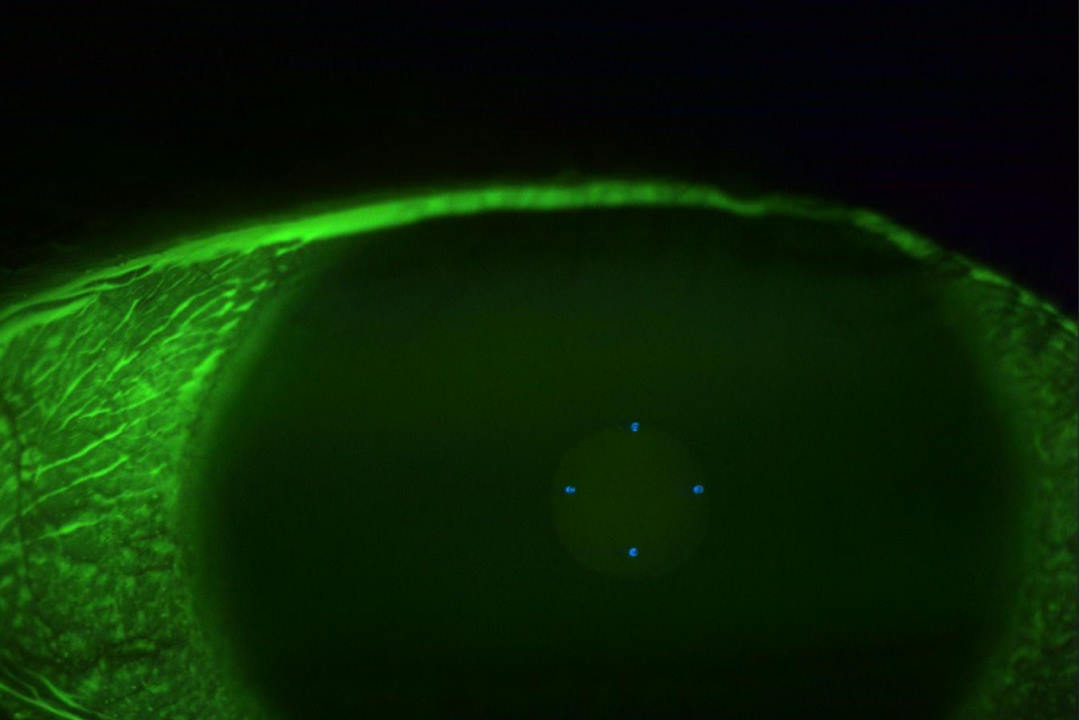
The patient was a 30-year-old male office worker I’d been managing for six months for evaporative dry eye disease. He had persistent corneal staining (Fig 1.) and suffered from significant corneal discomfort. In addition to consistent home therapy with warm compresses, omega-3 supplements and ocular lubricants, he received treatment with thermal pulsation using LipiFlow and quantum molecular resonance (QMR) with Rexon-Eye. Although his symptoms improved slightly with this treatment regimen, the corneal staining remained and he continued to experience significant discomfort.
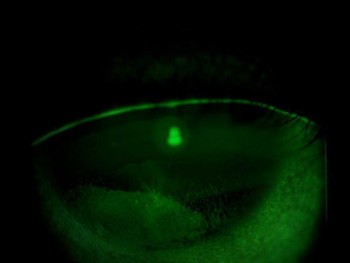
Fig 1. Fluorescein slit lamp image of the right cornea at
presentation
When patients do not make significant progress after being on such a comprehensive treatment plan, a reassessment of their environment can shed some light on the situation. In this case, the patient’s occupation appeared to be the main hurdle to his ocular surface recovery due to his prolonged digital screen use. The 2023 TFOS Lifestyle Report discussed in detail the risks of digital devices to the ocular surface¹. It names digital eye strain as a contributing factor to dry eye and provides a list of management recommendations, including omega-3 supplementation, regular breaks and blinking, as well as reducing computer work to fewer than four or five hours a day. Many of these recommendations were adhered to in this case, but the patient could not reduce his digital screen time due to his occupational requirements.
This is where scleral lenses can be advantageous. They protect the ocular surface from the effects of digital screens while providing continuous lubrication. The earlier TFOS DEWS II report placed scleral lenses in the third stage of its management algorithm², although a more recent review argued there may be benefits from using scleral lenses earlier in the treatment heirarchy³. There’s evidence that scleral lenses eliminate the direct ocular surface impacts of4, 5,6, 7.
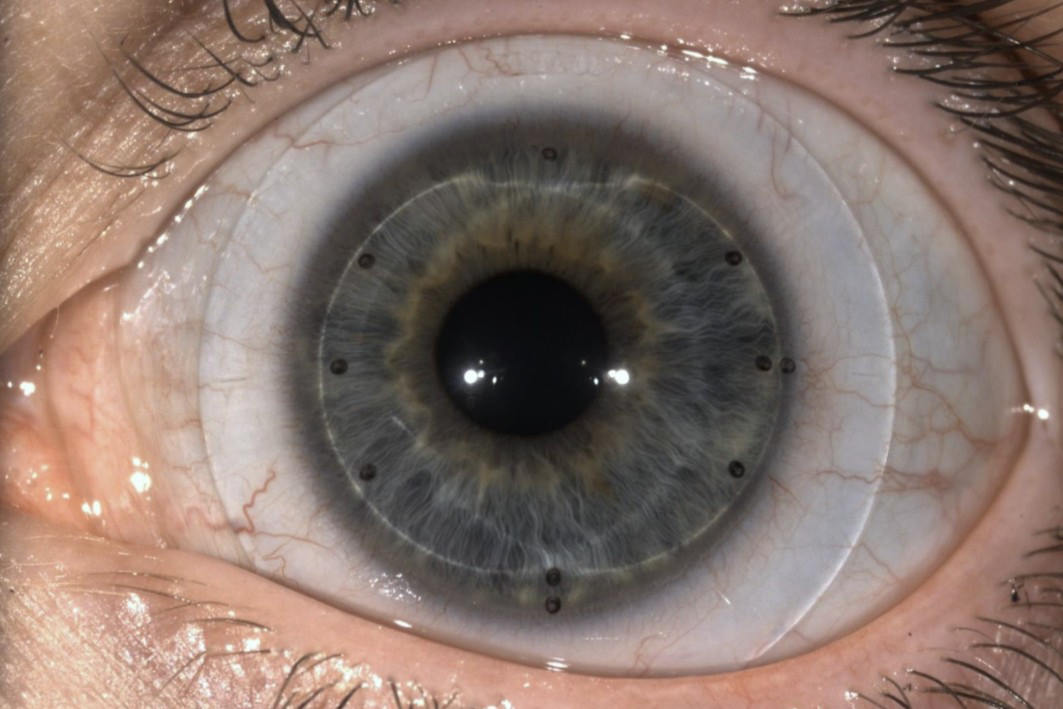
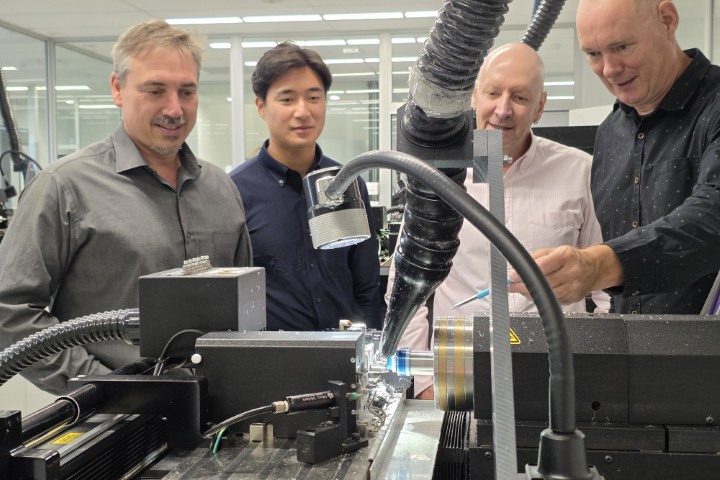
After a discussion with the patient, the decision was made to proceed with scleral lens fitting. I prefer to use the sMap3D device for scleral lens fitting as it allows for a fully customisable lens design over 360° (Figs 2 and 3)8. After fitting and dispensing the sMap3D scleral lenses, the patient was asked to start wearing his lenses while using his computer at work.

Fig 2. Simulation of the patient’s right scleral lens design based
on the 3D model of his eye

Fig 3. OCT scan of the lens on the eye
Within one day, his corneal staining improved dramatically from grade four to grade two in the right eye and from grade two to grade one in the left eye. In less than one month the corneal damage in both eyes had fully resolved (Fig 4). The patient was able to wear the lenses for up to eight hours a day at work and his eyes felt comfortable – for the first time in six months!
This case demonstrates the impressive capability of scleral lenses in cases of dry eye disease where there is persistent corneal staining linked to digital device use. The indications I use for fitting dry eye patients with scleral lenses are: prolonged digital device use (more than four hours a day) and non-responsive to other dry eye treatments. In essence, I place scleral lenses later in the treatment hierarchy, after exhausting the conventional routes.
References
1. Wolffsohn JS, Lingham G, Downie LE, Huntjens B, Inomata T, Jivraj S et al. TFOS Lifestyle: Impact of the digital environment on the ocular surface. Ocul Surf. 2023;28:213-252.
2. Jones L, Downie LE, Korb D, Benitez-Del-Castillo JM, Dana R, Deng SX et al. TFOS DEWS II Management and Therapy Report. Ocul Surf. 2017;15(3):575-628.
3. Qiu SX, Fadel D, Hui A. Scleral Lenses for Managing Dry Eye Disease in the Absence of Corneal Irregularities: What Is the Current Evidence? J Clin Med. 2024;13(13):3838.
4. Khan M, Manuel K, Vegas B, Yadav S, Hemmati R, Al-Mohtaseb Z. Case series: Extended wear of rigid gas permeable scleral contact lenses for the treatment of persistent corneal epithelial defects. Cont Lens Anterior Eye. 2019;42(1):117-122.
5. Theophanous C, Irvine JA, Parker P, Chiu GB. Use of Prosthetic Replacement of the Ocular Surface Ecosystem Scleral Lenses in Patients with Ocular Chronic Graft-versus-Host Disease. Biol Blood Marrow Transplant. 2015;21(12):2180-2184.
6. Alshami S, Bradley EA, Nau CB, Schornack M. Outcomes of scleral lens therapy in patients with neurotrophic keratopathy at a tertiary referral center. Invest Ophthalmol Vis Sci. 2018;59(9)1795.
7. Qiu S, Boshnick E. Case Report: Scleral Lens Management in a Case of Neurotrophic Keratitis Caused by Acoustic Neuroma. Clinical Insights in Eyecare. 2024;2(1).
8. Mahmoud R. Scleral lenses in DED management Sep 27 2021: https://nzoptics.co.nz/live-articles/scleral-lenses-in-ded-management/.

Ryan Mahmoud is a therapeutic optometrist who specialises in dry eye, specialty contact lens fitting and myopia control, and owner of Auckland independent optometry practice, NVision Eyecare.