Getting to grips with VR and AR’s potential in eyecare
Some time ago I had the chance to dip my toes into The Optical Metaverse, home to, among other things, the first virtual optical shop. The experience nudged my thoughts towards the potential for virtual reality (VR) and augmented reality (AR) in eyecare and how it can enhance everything from education to marketing.
I sought the assistance of Dr Irina Yakubin, a US-based primary-care and low-vision optometrist with experience working in the virtual world; and Dr Phil Turnbull, a senior lecturer with the School of Optometry and Vision Science (SOVS) at the University of Auckland who develops VR tools to assist optometry students.
VR and AR are already here
So what’s the difference between VR and AR?
VR immerses you in a completely artificial computer-generated world, usually by wearing a headset, whereas AR is a hybrid experience where you see and interact with the real world while additional digital content is superimposed over it. This is usually achieved with a smartphone, tablet or by wearing special smart glasses (with Snap’s depth-sensing AR filters for example).
VR and AR technologies have been around for decades, but their use has been hampered by technology limitations. The 2010s was a significant milestone, with the introduction of VR headsets such as the Oculus Rift and the advent of smartphones and tablets featuring AR experiences, such as the worldwide gaming phenomenon Pokémon GO.
Today, it seems VR and AR touch just about every part of our lives, being widely used in gaming, entertainment, marketing, education, healthcare and the military. Their applications are far-reaching, including everything from supporting children with attention deficit hyperactivity disorder to allowing people to ‘experience death’ via Shaun Gladwell’s Passing Electrical Storms, an ‘extended reality’ exhibition at Melbourne’s National Gallery of Victoria which guides you through a simulated ‘de-escalation of life’, from cardiac arrest to brain death!
VR and AR in eyecare
While the first forays into using VR and AR in the optical world for marketing (such as The Optical Metaverse’s virtual optometrist appointments) have been made, there’s still a long way to go, says Yakubin, with the potential in patient and student education particularly exciting. “VR can be used to simulate eye conditions for patient education. For instance, there’s been a recent uptick in TikTok videos showing how someone sees if they are a -1.00D myope versus if they are a -6.00D myope. Using VR for patient education can be especially helpful when you have a parent who is trying to understand their child’s eye condition.”
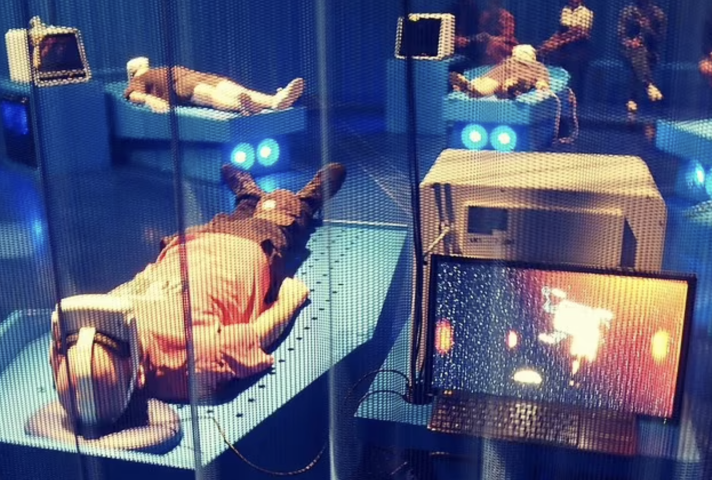
Artist Shaun Gladwell’s VR experience, Passing Electrical Storms, guides participants through a simulated deescalation of life, from cardiac arrest to brain death. Credit: Instagram/nasrita
VR can also help train the next generation of eyecare professionals, says Dr Yakubin. “VR, in combination with AI, can be used to create simulations to help improve diagnostic and practical skills.” Many of these things are already happening across Australia and New Zealand with the aim of improving clinical skills, decision-making and patient care. Trainee eye surgeons at the University of Auckland and Flinders Medical Centre in South Australia, for example, train on EyeSi VR simulators, allowing them to practise surgical skills on virtual eyes using a computer-connected microscope in a risk-free environment, while the University of Sydney ran two microsurgical courses in early 2023 enabling first-year RANZCO trainees to experience some EyeSi simulator time. Meanwhile, SOVS students have improved their real-life assessment test scores by 28% since the introduction of a virtual patient, the brainchild of Dr Turnbull, and the Royal Victorian Eye and Ear Hospital in Melbourne recently hosted Geneye, a fully immersive VR training event for trainee and current ophthalmologists.

Dr Irina Yakubin
While Dr Yakubin hasn’t used VR clinically, she says she saw the benefits first-hand during her optical training. “When I was at a low vision clinic, VR devices like the Vision Buddy and Olleyes were used to help patients improve their quality of life. These devices typically recreate our reality as a digital twin that the patient’s visual system can process.”
Aria Research, a Sydney-based startup, is undertaking a clinical trial of bionic glasses which allow blind and low-vision users to experience an immersive and detailed perception of their immediate environment in real time. Having reported extremely positive results, the company says the glasses will be manufactured in Australia and expects a 2025 launch.
VR can also be used for vision therapy to help train patients with strabismus, convergence insufficiency, amblyopia and possibly even depth-perception issues, in addition to sports vision training to improve hand-eye coordination and reaction time, says Dr Yakubin. Many vision specialists on both sides of the Tasman are currently using these VR training programmes to successfully treat amblyopia in children, as well as those suffering from traumatic brain injuries, she says.
The risks of too much VR
With prolonged VR use, however, patients can experience cybersickness, with symptoms including eyestrain, headache and nausea, says Dr Yakubin. “This might be linked to our ocular and vestibular systems working out of sync, but research is currently underway to better understand and combat what’s actually happening.”
Lark Optics is one such company investigating these phenomena. In response to a Bloomberg article citing US soldiers suffering “mission-affecting physical impairments” after using Microsoft’s HoloLens AR headset, Lark developed a lens to addresses the depth mismatch created when switching focus between the real and augmented world. The company says it plans to sell the resulting glasses, which project images directly onto the user’s retina, to the original AR equipment manufacturers.
Considering the long-term effects of VR headset use, although the jury is still out, Dr Yakubin says use, especially in children, should be approached with caution.
Known for his extensive VR research and development work, Dr Turnbull agrees, saying that while an adult logically knows to stop wearing a headset if things don't feel right, children will often continue to use it for extended periods. As an interesting aside, Dr Turnbull says he was approached by a multinational to discuss what issues to expect when releasing a novelty VR-type experience targeted towards children. It was never released, he says.

Dr Phil Turnbull
Kaimara et al’s systematic review of 85 VR studies from 2010-2020 showed findings were contradictory when it comes to risks for children and adolescents. The main physical concerns raised were the impact on children’s immature visuomotor system, as well as adverse effects on their accommodation, vergence, stereoscopic vision and hand-eye coordination. They also concluded, however, that these adverse effects were connected to unrestricted and unsupervised VR use in children.
With the long-term effects unknown, Dr Yakubin says she feels the eyecare industry must remain vigilant in keeping up with VR and AR research and better address ocular hygiene and visual eyestrain issues with patients. “Not just the 20-20-20 rule or the newer alternative of five-minute breaks every hour, but also the importance of complete blinking and correct viewing distances for digital devices.”
After reviewing 77 studies evaluating the growing use of VR/AR in ophthalmology, for training, diagnosis and patient treatment, Mina Iskander et al¹ concluded eyecare is well suited for the use of VR/AR. “We believe that time will indeed foster further technological advances and lead to widespread use of VR/AR in routine ophthalmic practice.”
Reference
- Iskander M, Ogunsola T, Ramachandran R, McGowan R, Al-Aswad LA. Virtual reality and augmented reality in ophthalmology: a contemporary prospective. Asia Pac J Ophthalmol (Phila). 2021 May-Jun 01;10(3):244-252

Renee Lunder is an Australian freelance journalist and proud specs wearer.