Nursing insights and outlooks at AONA 2025
This year’s Australian Ophthalmic Nurses Association (AONA) Congress began with a warm welcome from AONA president Dr Heather Machin and local AONA representative Rose Knowles. The day, packed full of a range of speakers and subjects, attracted 200 nurses. With such a strong programme and many highlights, this is just a snapshot of some of mine.
Fred Hollows Foundation’s Papua New Guinea (PNG) ophthalmic nurses Isabella Mou and Getruth Bare made us all realise, despite the challenges we face, ophthalmic nursing in PNG is a totally different (eye) ball game. Bare discussed surgical outreach programmes to meet the needs of a large population spread over a geographically diverse area. (Look at a map of PNG to see what ‘remote’ really means.) Walking or canoeing for days to get to a clinic appears to be the norm for most of the individuals who attend the outreach clinics. For the ophthalmic team who set up those clinics, it’s also a hard slog. Fred Dagg’s song We Don’t Know How Lucky We Are kept running though my head!
Mou spoke about the advanced diploma in eyecare training to meet the needs of ophthalmic patients and outlined many of the barriers to care. The diploma is divided into theoretical, practical and supervised placements and includes refracting and prescribing spectacles for when you work in outreach clinics. That’s because, as expected, a high percentage of poor vision is secondary to refractive issues.
Barriers to care were also discussed by Amanda Davis, chair of the International Agency for the Prevention of Blindness (IAPB) in the Western Pacific. With over 1 billion people worldwide having no access to eyecare, Davis explained IAPB’s aim is to elevate sight as a political issue to obtain social and economic support. Another reminder of how lucky we are.
Engaging with the local community to close health gaps was the driver of a culturally safe patient information poster that Peter Mitchell discussed. Mitchell, a registered nurse and programme manager for the Indigenous Remote Eye Service (IRIS), is based in Australia’s Northern Territory. With planned cataract clinics having high numbers of patients missing appointments, IRIS developed a poster with images and in local languages to explain the cataract surgery process, in consultation with First Nation representatives and other healthcare providers. Explaining the pre-op clinic review, the theatre area and then post-op review, the poster is a great way to try and reduce fear, improve attendance and meet patients’ needs.
Meeting patients’ needs was also the focus of Dr Zali O’Dea's talk. The founder, director and principal counsellor and educator at Karibu Anawim, she presented on the psychological needs of patients with facial disfigurement, having established Karibu Anawim (welcome to the way of victory) to help train health carers to support these patients and their families. Karibu Anawim even provides services for international clients, thanks to Zoom, while karibuanawim.com offers free downloadable self-help guides. Dr O’Dea also movingly explained her own experiences of living with a third-nerve palsy, which alters her appearance from “the norm”, and the personal challenges she and her daughter have encountered because of this.
Seeing Differently
More insight into helping vision-impaired individuals was presented by Royal Society for the Blind executive director Damian Papps, who explained the Seeing Differently group. Like Blind Low Vision NZ, it provides low-vision services in South Australia, but since the word ‘blind’ often puts people off, Seeing Differently fits the bill, said Papps. As he gave an overview of how they help individuals with sight loss, I found myself envious of the National Disability Insurance Scheme funded by Australia’s Federal Government, as it certainly helps Seeing Differently provide support.
But even if funds are low, there are still tips we can pass on to our patients with low or impaired vision. Seeing Differently optometrist Christina Ly suggested thinking of three main themes – bright, bold and big – and emphasised the importance of good lighting. She also discussed the role of contrast, especially for patients with macula pathology experience. And yes, size does count if you have reduced vision. As well as showing us how to access a free cell phone magnifying app, Ly brought along a guide dog, which was a delight.
There were also presentations on meeting nurses’ needs, including – you guessed it – education. Joanna McCulloch, clinical nurse ophthalmology consultant at Sydney Eye Hospital, spoke about setting up (and the difficult job of sustaining) the ophthalmic nurse education programme in NSW, which now has support from the University of Notre Dame. The need to develop online learning to make the programme more accessible was also discussed – this year’s University of Auckland ophthalmic nursing specialty paper also had an online delivery mode.
Jessica Raab, director of medical education at Corza Ophthalmology, US, gave an eye-opening presentation on taking care of ophthalmic instruments. She highlighted their delicacy, explaining the master-craftsman skill that goes into making an ophthalmic instrument and reminded us how easily they can be damaged. Basic safe handling and working with your area’s sterile supply staff is vital, she said. Raab showed a few worrying images with ophthalmic instruments dumped in with orthopaedic instruments. She urged us to check how our instruments are transported to the sterile supply team and what happens to them once there. As always, clear communication and education are key.
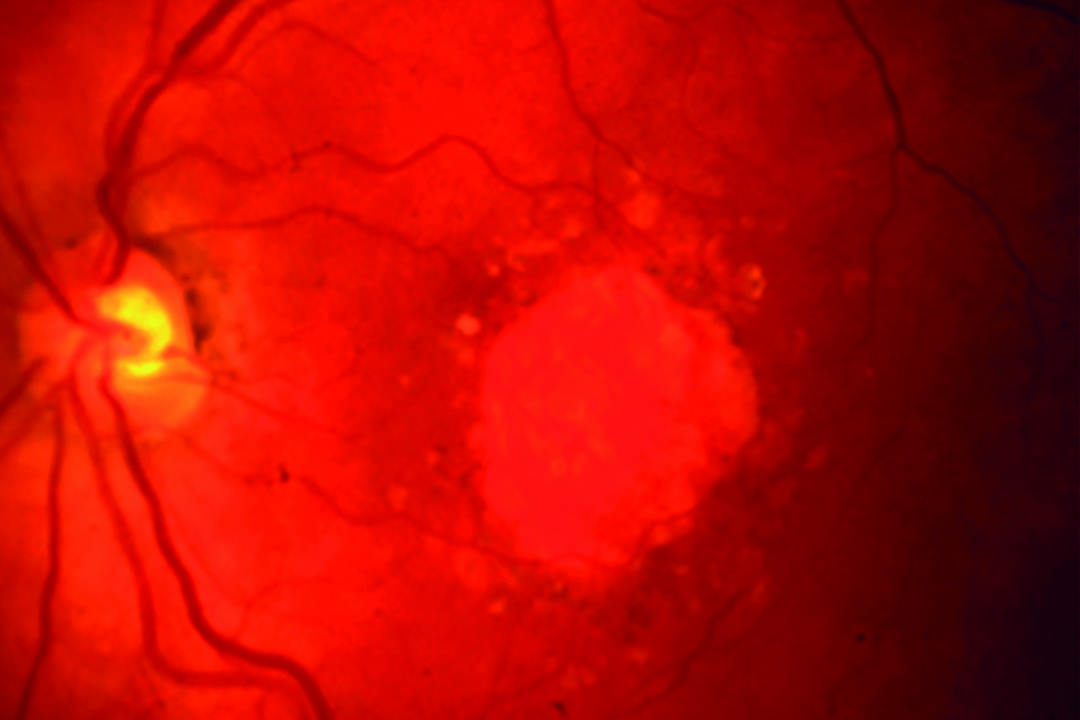
Keeping with the education theme, Gold Coast University Hospital interventional clinical ophthalmology nurse consultant Carmen Newman discussed the education pathway she went through to establish a nurse-led intervention service for the treatment of macular diseases. Unsurprisingly, she underlined the importance of support from senior staff, but also of one’s nursing colleagues. Such support was reinforced in a presentation by Nicole Wyatt and Tierney Mikolaj in their role as clinical nurse specialists at the Day Ophthalmology Unit, Flinders Eye Centre. They outlined the superpowers one learns, including the power of seeing in the dark (retinal surgery, anyone?).
I must also highlight Vision Hospital Group’s national director of nursing Kylie Bennett’s thought-provoking ‘Sustainability in healthcare’ presentation. Given the waste we generate, especially in the operating theatre, ‘sustainability’ and ‘health’ might seem contradictory but, as Bennett explained, we need to look at how to aim for sustainability. She reminded us of the importance of factoring in environmental impact when, for example, procuring instruments and products, and looking at sustainable transport plans to reduce emissions. This includes how your products are delivered to your unit and also how you get to work. In New Zealand, most of our products are manufactured and come from overseas, but ask your suppliers and reps what can be done to reduce packaging for a lighter load to transport. I could discuss this all day, but I will finish by thanking all the presenters for a most enlightening and informative day and saying to the AONA organising committee: bravo, job well done!
Olga Brochner is a clinical nurse specialist in ophthalmology with Te Whatu Ora, based at Greenlane Eye clinic and was AONA 2024's keynote speaker.