O=Mega21: virtually unstoppable
From 2-4 September 2021, many of us had anticipated being in metropolitan Melbourne, enjoying some socialising, a trade fair and some CPD education. Instead, the Covid-19 lockdowns blighting New South Wales and New Zealand led to O=Mega21’s inevitable pivot to online.
Thankfully, organisers harnessed the strengths of this virtual medium, promoting engagement and interconnectedness by using break-out rooms during some of the live presentations. This gave us a chance to connect with other optometrists, hear their experiences and sometimes even discuss learning points with speakers. One grumble, however, is that the lectures were only accessible online for two weeks following the conference; sometimes it’s nice to be able to revisit the presentations, especially when they address new frontiers!
A selection of clinical pearls
On the subject of ocular antimicrobials, Deakin University’s professor of vision science Dr Alex Gentle and Queensland optometrist and lecturer David Foresto were as entertaining and engaging as ever, cautioning us to be mindful of antibiotic resistance, even with topical agents. When it comes to using prophylactic topical antibiotics with topical corticosteroids (for instance, in treating marginal keratitis), start with a loading dose, then drop to your recommended therapeutic dosage, but, rather than tapering, advise your patient to discontinue the antibiotic two days after the cornea has re-epithelialised. This dosing limits the development of antibiotic resistance while still giving prophylactic care. Another interesting point arising from their case studies was that although topical ciprofloxacin is often our go-to for good gram-negative coverage, it makes patients more prone to delayed epithelial healing when compared to topical ofloxacin1.

Dr Alex Gentle and David Foresto
Brien Holden Vision Institute executive director Dr Tim Fricke explored new evidence relevant to paediatric optometry and discussed the importance of recognising evidence gaps. While we have become accustomed to defining amblyopia as vision loss in the absence of visible pathology, a new study has demonstrated a visible difference between amblyopic and non-amblyopic eyes with OCT angiography. Amblyopic eyes had abnormal macular microvasculature, represented by decreased foveal avascular zone (FAZ) circularity, and increased vessel diameter index2. These findings were associated with the subject’s best corrected visual acuity (BCVA). Dr Fricke’s literature review studying the mechanisms by which outdoor time prevents myopia was also interesting, albeit with no conclusive evidence as yet. Vitamin D could play a role in the process3, as could dopamine.
Seeing both sides
Also interesting was a discussion about the role of facial asymmetry in increasing the demands on fusion when assessing a child’s risk of developing strabismus. Personally, I have often overlooked making a gross assessment of my patient’s facial symmetry and have only recently become aware of how prevalent the phenomenon is from recent social media trends (namely TikTok) that highlight a user's facial symmetry (or lack thereof!), as well as the rise of facial dysmorphia resulting from frequent Zoom meetings!
Contact lens specialist optometrist Richard Lindsay discussed some interesting paradigm shifts in contact lens management of keratoconus, one of which was using higher modulus silicone hydrogel contact lenses (such as PureVision2 toric and Air Optix toric) as optical correction for early keratoconus because they can achieve less spectacle blur than rigid corneal lenses. There’s also an increased use of corneoscleral lenses (eg. Rose K2 XL) due to their higher Dk/t when compared to scleral lenses, decreased limbal pressure (because the lens bearing is shared between the sclera and cornea) and increased tear exchange without compromising visual acuity, comfort, or stability. This is especially the case for patients with inferiorly displaced cones, he said.
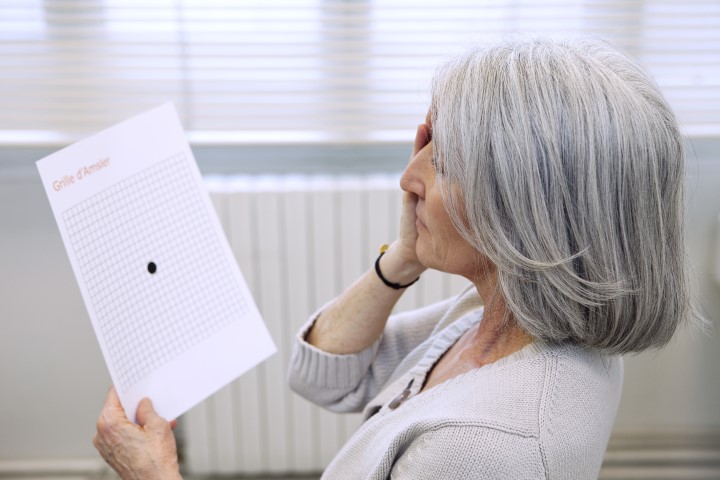
Masqueraders and medical retina
Melbourne retinal specialist Dr Nicholas Cheng reviewed some optical coherence tomography (OCT) acronyms that can help us identify at-risk patients. These were:
- SIRE (shallow irregular retinal pigment epithelium (RPE) elevation) for AMD: Often found in asymptomatic patients, a long and shallow elevation of RPE is caused by non-exudative macular choroidal neovascularisation (CNV). This fibrovascular tissue causes non-homogenous reflectivity of sub-RPE and irregularity of RPE. Identification of at-risk eyes can help us adjust our review schedule and make us more likely to pick up early manifestations of complications, in this case exudative CNV
- DRIL (disorganisation of the retinal inner layers) for diabetic retinopathy: Although most patients with diabetic macular oedema and good baseline VA can be managed with observation, those with DRIL, hyper-reflective foci, and a disrupted ellipsoid zone at baseline are at an increased risk for VA loss
Dr Cheng also discussed the growing epidemic of the great masquerader syphilis in Australia; its rate has more than doubled between 2004 and 2017. It can occur at any age and has three stages of presentation. Secondary syphilis can occur from two months to three years after primary infection and can present as an inflammation of any layer of the eye anterior – uveitis, retinitis, chorioretinitis and papillitis being the most common. The tertiary presentation of the infection has neurological manifestations. So the takeaway here is to make sure you dilate every single uveitis patient to examine for retinitis, chorioretinitis and papillitis and request a blood test for syphilis markers. Venereal disease research laboratory test (VDRL), rapid plasma reagin (RPR) and rapid syphilis tests (RST) are non-specific markers, while fluorescent treponemal antibody test absorption test (FTA-Abs) and microhemagglutination assay (MHA-TP) are specific. In an international survey of 100 uveitis specialists, 80 of them tested every uveitis patient for syphilis, added Dr Cheng.
Dr Nicholas Cheng
Melbourne-based Professor Allison McKendrick and Associate Professor Tissa Wijeratne also discussed syphilis, but as a relevant differential diagnosis for tonic pupils with light-near dissociation (Argyll Robertson pupils). Providing a great refresher on neuro-optometry, their rule of thumb was that bilateral presentations were more likely to be caused by systemic infections and unilateral tonic pupils by a space-occupying lesion.
Glaucoma resources
ACO’s lead ocular disease service optometrist Janelle Scully and Melbourne-based optometrist Laura Carson shared some interesting case studies about glaucoma and the anterior eye, and offered us a reminder to check the Optometry Board AHPRA (OBA) guidelines for use of scheduled medicines for referral requirements for the confirmation of diagnosis and ongoing management of glaucoma. Other useful resources were Optometry Australia’s clinical practice guide for glaucoma and the National Health and Medical Research Council (NHMRC) glaucoma guidelines.
Overall, O=Mega21 rescued victory from the jaws of defeat by playing to the strengths of the online medium. It was filled with invaluable recommendations with clinical application. I’m already looking forward to next year’s!
References
1. Patel GM, Chuang AZ, Kiang E, Ramesh N, Mitra S, Yee RW. Epithelial healing rates with topical ciprofloxacin, ofloxacin, and ofloxacin with artificial tears after photorefractive keratectomy. J Cataract Refract Surg. 2000 May;26(5):690-4
2. Wong ES, Zhang X, Yuan N, et al. Association of Optical Coherence Tomography Angiography Metrics With Detection of Impaired Macular Microvasculature and Decreased Vision in Amblyopic Eyes: The Hong Kong Children Eye Study. JAMA Ophthalmol. 2020;138(8):858–865.
3. Lingham G, Mackey DA, Lucas R, et al. How does spending time outdoors protect against myopia? A review. British Journal of Ophthalmology 2020;104:593-599.

Australian-based optometrist Layal Naji is a lecturer of optometry at the University of Canberra and co-founder of the outreach optometry clinic at the Asylum Seekers Centre in Newtown, Sydney.