Oculoplastics update
Evaluation of the risk of hypertrophic scarring and keloid following eyelid procedures
L Anderson et al
Aesthet Surg J, Aug 2023, p820-829
Review: This systematic review covered all articles mentioning hypertrophic scarring and a variety of oculoplastic surgery terms. The outcomes were:
- 107 total abstracts, with only 34 full texts available
- 20 articles made no mention of any hypertrophic or keloid scarring
- 13 studies mentioned hypertrophic scarring in the eyelid (36/3,650 patients)
- 1 person developed lid keloid scarring after tarsorrhaphy (post-burn)
The review was limited as it was impossible to capture all oculoplastic studies reporting outcomes, the included studies seeming quite low in number and the fact hypertrophic scarring may not be a commonly reported outcome.
Comment: This mirrors my experience as the eyelid tends to be a very forgiving area in terms of scarring. This is useful in counselling patients about real-world surgery risks, as we can confidently tell them we do not routinely expect hypertrophic or keloid scarring, even in those at risk of keloid scars elsewhere.
Eye trauma in mixed martial arts and boxing
C-C Chang et al
Ophthalmic Plast Reconstr Surg 40(1):p 75-87, Jan/Feb 2024
Review: This retrospective cohort review extracted data from boxing and mixed martial arts (MMA) competitions from the Nevada Athletic Commission (NAC) between 2000 and 2020. These data included details of competitions, contestants, outcomes and injuries. The outcomes were:
- 1,539 boxing injuries and 1,442 MMA injuries were recorded
- Boxing had higher eye injury rates compared to MMA (p< 0.0001), with an odds ratio of 1.268 (95% CI, 1.114-1.444)
- Eye trauma represented 47.63% of boxing injuries and 25.59% of MMA injuries, with periocular lacerations being the most common eye injury in both. Orbital fractures represented 17.62% of eye injuries in MMA and 3.14% in boxing contests
- Retinal injuries were recorded in 2-3% of each sport, with 3.27% being glaucomatous in boxing alone
- MMA contestants had an odds ratio of 1.823 (95% CI, 1.408-2.359) for requiring physician evaluation following an eye injury, compared with boxing
- MMA also had a higher risk of associated face and body injuries
- Being the losing fighter and the number of rounds were associated with increased odds of injuries
The review was limited by being retrospective and including just one state’s athletic commission.
Comment: As a sports fan, I found this to be an interesting study, evaluating the relative risk of eye injuries in two combat sports. Although boxing had a higher risk of eye injuries, it seems the injuries are worse and distributed more around the body in MMA, since a wider range of attacks are allowed. There was also an increased risk of orbital fractures and the need for physician evaluation in MMA, likely related to the use of smaller, less padded gloves causing higher energy transmission. Although MMA has significantly fewer rounds and total duration of combat, it affords greater damage, concentrated into a shorter time, compared with boxing.
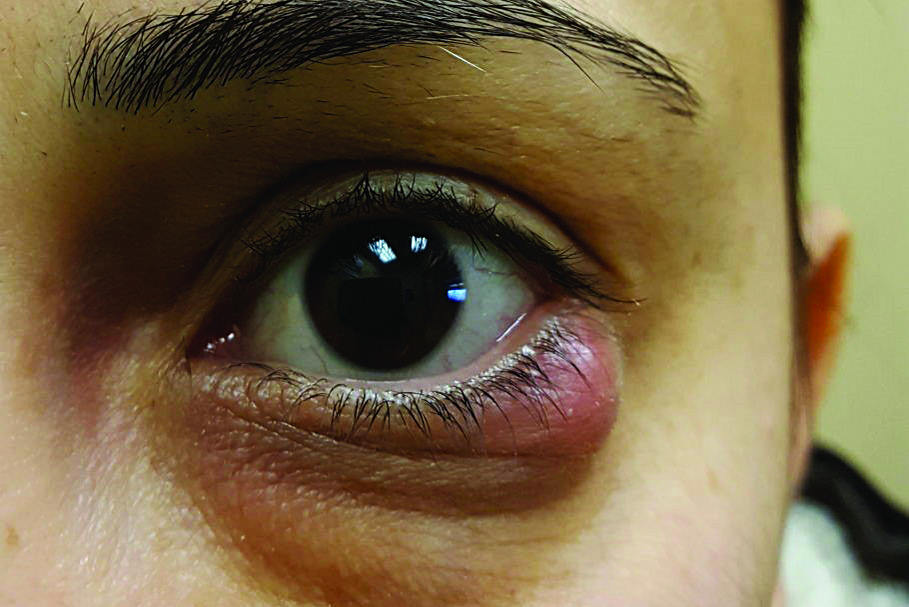
Novel treatment of chalazion using light-guided-tip intense pulsed light
Y Zhu, et al
Sci Rep. 2023 Jul 31;13(1):12393
Review: This prospective non-randomised study included 95 eyes with inflamed chalazion that did not respond to one week of conservative treatment and 95 eyes in the control group. Those suitable were given intense pulsed light (IPL) therapy with meibomian gland expression in repeat sittings until the chalazion had improved by 80%, while the control group had incision and curettage until the cyst had reduced by 80%. Both groups were supported by topical antibiotic and steroid treatment. The outcomes were:
- The IPL group responded to treatment nearly as well as the control group, with a statistically significant reduction in size of lesions (although the control group end result was slightly better)
- Mean number of IPL treatments: 4.0 (range: 3-6)
- Mean number of incision and curettage: 2.1 (range: 1-4)
- At six months, 14.7% of the IPL group had recurred, while 37.9% of the control group had a recurrence
- Treatment was well tolerated, with skin redness/burning sensation in 40% of IPL patients, which was resolved for all with five minutes of cold compresses
- 21.4% of IPL patients failed and went on to have incision and curettage
- Secondary measures, such as tear break-up time, meibomian gland quality, dropout and expressibility, all improved in the IPL group post-treatment and were not improved in the control group
The study’s limitations included it being small and non-randomised, the long duration of treatment (IPL treatments took at least 12 weeks, while surgery was much faster) and being limited to Fitzpatrick skin types 1-4 (those who can tolerate IPL). All patients also had some steroid during the study, which was perhaps responsible for some of the improvement.
Comment: We are all aware of the increasing role of IPL in dry eye and blepharitis management and this was an interesting study on its application in acute chalazion. Although this study was limited, encouraging trends were highlighted, such as resolution of chalazion, as well as improvement in other tear film parameters. Recurrence was also lower in the IPL group. We currently offer Optilight IPL in our dry-eye clinic and this may be an alternative option for patients who are averse to surgery or more invasive therapy.

Dr Sid Ogra is a oculoplastic and cataract surgeon working at Auckland Eye and Manukau SuperClinic and an honorary senior lecturer at the University of Auckland, with a specialist interest in functional and cosmetic surgery, vision correction and pterygium surgery.