Orally delivered drugs in clinical trials for DR: looking into the future
Intravitreal anti-vascular endothelial growth factor (anti-VEGF) injections, laser panretinal photocoagulation and intravitreal corticosteroid implants are clinically used to resolve diabetic macular oedema (DMO), the most common cause of vision loss in diabetic retinopathy (DR) patients. However, these are only indicated for patients who have developed sight-threatening DR. They are not used prophylactically, do not reduce the risk of disease progression and may need to be repeatedly administered if oedema recurs. In the hope of discovering novel therapeutics to halt DR progression, several clinical trials are now underway. Metformin and fenofibrate, which are well-known diabetes medications, have shown encouraging clinical results in slowing DR progression.
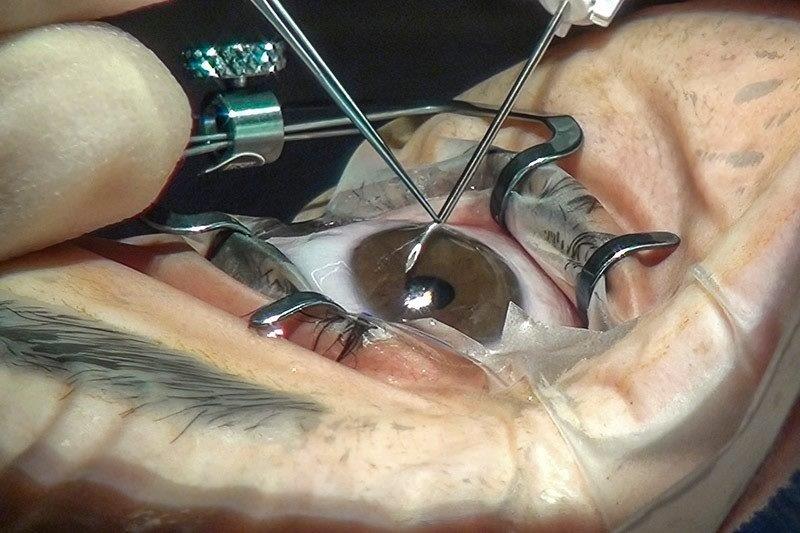
VEGF is a major cytokine that promotes angiogenesis and vascular permeability in DR; therefore, injections of anti-VEGF agents into the vitreous have been used to stop active vascular leakage. Commercially available anti-VEGF agents include bevacizumab, pegaptanib, ranibizumab, aflibercept, conbercept, brolucizumab and abicipar pegol. As the patents of some of the currently used anti-VEGF agents approach expiry, several biosimilars (defined as “a biological product that is shown to be highly similar in terms of its quality, safety and efficacy to an already licensed reference product” by the World Health Organization) have also recently entered the market¹. Common adverse effects associated with intravitreal anti-VEGF injection include subconjunctival haemorrhage, eye pain, elevated intraocular pressure and floaters, while more serious adverse events such as cataract formation, endophthalmitis and rhegmatogenous retinal detachment are uncommon².
One of the main limitations for anti-VEGF therapy is that repeated administration is required, increasing treatment costs. Therefore, new DR therapeutics with longer lasting effects, which reduce the frequency of injections, have been developed. One such drug is faricimab, a combination drug that inhibits not only VEGF-A but also angiopoietin-2, which enhances vascular stability³. Phase 3 clinical trials for faricimab assessing its efficacy and safety in patients with DMO have been completed and an active, non-recruiting phase 3 trial is ongoing to evaluate its long-term safety and tolerability. Phase 4 trials which examine its efficacy as a fixed dose compared to ‘treat and extend’, in treatment-naïve patients and for DMO patients (with limited response to aflibercept) are also underway.
Alternatives to anti-VEGF therapy?
In 2014, dexamethasone was approved by the US Food and Drug Administration (FDA) for DMO treatment. It allows the active ingredient, dexamethasone, to release into the vitreous cavity over time with efficacy lasting up to six months. However, side effects include a high risk of steroid-induced elevation in intraocular pressure, which increases the risk of glaucoma and cataract formation, in turn reducing vision⁴. Besides dexamethasone, another corticosteroid sustained release formulation, a fluocinolone acetonide implant, is also on the market to treat DMO. Several phase 3 and 4 clinical trials confirmed efficacy and safety of Iluvien for DMO. The fact that corticosteroids can be used to treat DMO indicate that inflammation is involved, therefore it would be ideal to have a non-steroidal anti-inflammatory treatment which does not induce intraocular pressure elevation and cataract formation.
Other anti-inflammatory drugs
Activation of the nucleotide-binding oligomerisation domain- (NOD-) like receptor (NLR) protein 3 (NLRP3) inflammasome pathway, a part of the innate immune system which becomes overactivated causing systemic low-grade inflammation, has been suggested to contribute to DR progression⁵. Currently, there are no clinically available DR interventions designed to target the NLRP3 inflammasome. However, medications routinely used to manage DR-associated risk factors have been shown to affect NLRP3 inflammasome activation in patients with diabetes. Moreover, novel anti-inflammasome therapeutics are also being investigated in clinical trials (Table 1).
Fenofibrate, a medication for controlling blood lipid levels, has been clinically proven to reduce DR progression and the necessity for laser panretinal photocoagulation⁶. Separate from its main function in managing dyslipidaemia, studies suggest that as a peroxisome proliferator‐activated receptor-alpha (PPAR-α) agonist, fenofibrate may ameliorate DR by inhibiting pro-inflammatory transcription factor nuclear factor kappa beta (NF-ĸB), VEGF production, apoptosis and reduce oxidative stress by upregulating superoxide dismutase⁷-⁹. A phase 3 clinical trial is currently recruiting to investigate fenofibrate’s effect on preventing DR progression.
Metformin, which has been used to control hyperglycaemia in patients with diabetes for many years, is also associated with a reduced risk of DR development and progression¹⁰. Although no study has directly investigated the effect of metformin on DR progression, it has been associated with reduced secretion of key inflammasome biomarkers, IL-1β and IL-18, by macrophages derived from the blood of patients with diabetes¹¹. It has also been found to inhibit inflammation, retinal cell death and choroidal neovascularisation in neovascular age-related macular degeneration, which, similar to DR, also involves retinal vascular leakage¹². As such, metformin’s anti-inflammatory effect is likely associated with inhibition of NLRP3 inflammasome activation. But further research is required to investigate these effects on DR progression. An early phase 1 trial is currently in the recruitment stage to compare DR progression among type 2 diabetic patients treated with metformin and insulin.
Several NLRP3 inflammasome inhibitors are also being investigated as potential DR treatments. Minocycline, a broad-spectrum antibiotic which has been shown to inhibit NLRP3 inflammasome activation at transcriptional and posttranscriptional levels¹³, is currently in phase 2 clinical trials. Tonabersat, a Connexin43 hemichannel blocker, suppresses inflammasome activation by obstructing adenosine triphosphate (ATP) efflux through open Connexin43 hemichannels. ATP efflux can induce inflammasome assembly and thus activation, therefore, tonabersat can potentially be an upstream blocker of the activated NLRP3 inflammasome pathway. It is currently being evaluated for its effect in DMO in a phase 2 clinical trial.
Evidence from clinical trials has shown that specific drugs (fenofibrate, metformin) appear effective in slowing DR progression independent of hyperglycaemic control. Several NLRP3 inflammasome inhibitors, including minocycline and tonabersat, are being investigated as novel therapeutics for DR in clinical trials. As such, activation of the NLRP3 inflammasome, which can initiate various downstream inflammatory cascades, is likely to be associated in the complexity of DR pathogenesis.
Alternative administration routes
The fact that different inflammatory pathways are targeted by novel therapeutics signifies the importance of inflammation as the key driving force of DR progression. Besides intravitreally administered drugs, novel orally delivered drugs for DR are also under development (Table 1). While intravitreal injections ensure that a drug quickly reaches the retina, it is an invasive procedure that needs to be repeated and must be done by trained personnel. In contrast, oral medications are more convenient, while their systemic effects can potentially benefit other complications of diabetes, such as nephropathy and neuropathy.
Conclusions
While anti-VEGF therapy has revolutionised the management of sight-threatening DR and DMO over the past decades, current clinical trials are exploring alternative approaches with a focus on preventive and anti-inflammatory therapies as well as sustained release options. Overall, it is crucial to strike the right balance between efficacy, administration frequency and patient convenience to achieve improved outcomes for individuals affected by DR.

Table 1. Orally delivered drugs in clinical trials for diabetic retinopathy (clinical trial information obtained from https://www.clinicaltrials.gov/)
References
1. Kapur M, Nirula S, Naik M, Future of anti-VEGF: biosimilars and biobetters. Int J Retin Vitr 2022, 8, 1-8.
2. Uludag G, Hassan M, Matsumiya W, Pham B, Chea S, Trong Tuong Than N, Doan H, Akhavanrezayat A, Halim M, Do D. Efficacy and safety of intravitreal anti-VEGF therapy in diabetic retinopathy: what we have learned and what should we learn further? Expert Opin Biol Ther 2022, 22, 1275-1291.
3. Khan M, Aziz, A, Shafi, N, Abbas T, Khanani A. Targeting angiopoietin in retinal vascular diseases: a literature review and summary of clinical trials involving faricimab. Cells 2020, 9, 1869.
4. Karti O, Saatci A. Place of intravitreal dexamethasone implant in the treatment armamentarium of diabetic macular edema. World J Diabetes 2021, 12, 1220.
5. Kuo C, Murphy R, Rupenthal I, Mugisho O. Correlation between the progression of diabetic retinopathy and inflammasome biomarkers in vitreous and serum - a systematic review. BMC Ophthalmol. 2022, 22, 238.
6. Keech A, Mitchell P, Summanen P, O'Day J, Davis T, Moffitt M, Taskinen M, Simes R, Tse D, Williamson E. Effect of fenofibrate on the need for laser treatment for diabetic retinopathy: a randomised controlled trial. Lancet 2007, 370, 1687-1697.
7. Inoue K, Kataoka S, Kawano S, Furukawa T, Lois N, Watanabe N. Fenofibrate for diabetic retinopathy. Cochrane Database Syst. Rev. 2019.
8. Abcouwer S. Direct effects of PPARα agonists on retinal inflammation and angiogenesis may explain how fenofibrate lowers risk of severe proliferative diabetic retinopathy. Diabetes 2013, 62, 36.
9. Jin L, Hua H, Ji Y, Jia Z, Peng M, Huang S. Anti-inflammatory role of fenofibrate in treating diseases. Biomol. Biomed. 2023, 23, 376.
10. Fan Y, Wu C, Lin J, Hsiung C, Liu H, Lai J, Yang C. Metformin treatment is associated with a decreased risk of nonproliferative diabetic retinopathy in patients with type 2 diabetes mellitus: a population-based cohort study. J Diabetes Res 2020.
11. Lee H, Kim J, Kim H, Shong, M, Ku B, Jo E. Upregulated NLRP3 inflammasome activation in patients with type 2 diabetes. Diabetes 2013, 62, 194-204.
12. Dang K, Wu T, Hui Y, Du H. Newly-found functions of metformin and treatment of age-related macular degeneration. Int J Ophthalmol 2021, 14, 1274.
13. Chen W, Zhao M, Zhao S, Lu Q, Ni L, Zou C, Lu L, Xu X, Guan H, Zheng Z. Activation of the TXNIP/NLRP3 inflammasome pathway contributes to inflammation in diabetic retinopathy: a novel inhibitory effect of minocycline. Inflamm Res 2017, 66, 157-166.

Charisse Kuo is a therapeutically qualified optometrist in the final year of her PhD at the University of Auckland (UoA). Her research involves the development of tissue-culture models using donor retinas and choroids to explore the mechanisms behind DR.

Associate Professor Ilva Rupenthal is the director of the Buchanan Ocular Therapeutics Unit (BOTU) in the Department of Ophthalmology at UoA.

Rinki Murphy is a professor of medicine at the University of Auckland, an endocrinologist specialising in diabetes and obesity at Auckland Diabetes Service, Greenlane, and clinical head of the Specialist Weight Management Service Te Mana Ki Tua at Te Whatu Ora Counties Manukau.

Dr Lola Mugisho is a senior research fellow and deputy director of BOTU. Her research involves developing pre-clinical models in which to test the efficacy of novel anti-inflammatory therapeutics for the treatment of age-related neurodegenerative diseases affecting the eye and brain.