Referral know how with Counties
Seeking to improve engagement and co-management of patients, Counties Manukau SuperClinic hosted an inaugural optometry open evening.
Inspired by private practices’ CPD evenings, Counties optometrists and organisers Deepa Kumar, Sandhya Mathew and Debra So said they hoped the event would clear up any questions referring optometrists may have and offer a better understanding of the patient journey at Counties. “The initial referral is the first important step of the patient journey into the hospital system and it does have a big impact on the timeliness of delivery of patient care,” said So. “Our hope is that if our referrers have a deeper understanding of how things work at our end, then that knowledge will help them in both forming an easy-to-triage referral and informing the patient of what to expect.”
Dr Graham Reeves, clinical head of department, kicked off the evening covering the patient flow at Counties and the context within which the clinic operates. The three-site clinic accepts 87% of its 12,000 annual referrals, he said. Dr Reeves encouraged referring optometrists to use HealthLink/Care Connect which helps the team prioritise patients while also supporting communication between the referring optometrist and Counties. After an initial nurse assessment, the patient is triaged by an ophthalmologist (or orthoptist for paediatrics) and is assigned priority 1-4 (P1a=acute, P1b <2 weeks, P2<6 weeks, P3<12 weeks, P4<16 weeks) or declined. The patient then receives an acknowledgement of wait listing and expected wait time. If eligible, the patient receives an appointment letter and text reminder when a clinic slot becomes available.
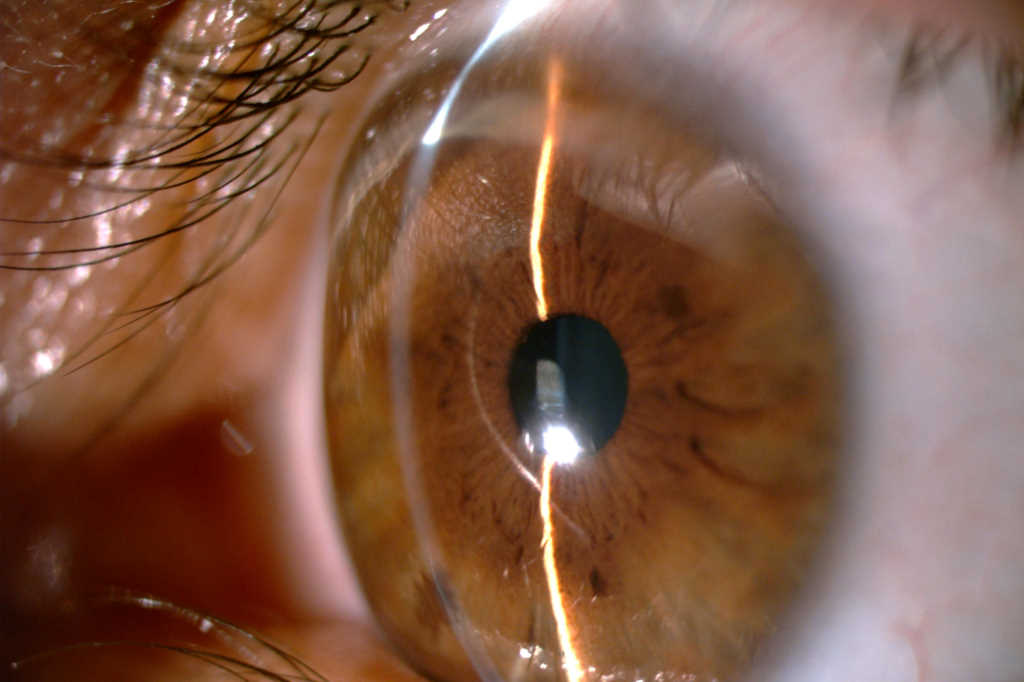
Keratoconus referrals
Next, So discussed keratoconus in paediatric patients, a common and growing concern in South Auckland. She advised optometrists to refer all paediatric keratoconus patients for crosslinking consideration. For adults, a documented progression is preferred unless the optometrist suspects there is a high risk of progression. A referral should include background atopy, eye rubbing and family history (Counties screen siblings as well); best spectacle-corrected visual acuity (BSCVA) and refraction; previous BSCVA, if possible, for comparison (showing evidence of progression); and topographies or keratometry readings, including previous results, if available. If the referring optometrist wishes to see the patient for contact lens fitting afterwards, or is referring to a colleague, this information should also be included, she said. “Co-managing these patients, we’d like to see community optometrists managing ocular allergies and reminding their patients to avoid rubbing their eyes. A comprehensive discussion with the patient about the condition can also help save chair time at our end. Lastly, we ask you to stress the importance of attending appointments.”
Glaucoma referrals: less is more
Prioritising glaucoma patients at Counties, Dr James Stewart highlighted the busy public setting and the real risk of missing important details if there’s too much information in the referral. “Too much stuff buries the important stuff,” he said.
A general medical history and drug history is only relevant if it’s pertinent to the referral problem, he said, adding that social details are helpful to include, for example if there’s a need for a translator or if there’s a dementia diagnosis. A good referral letter always accurately conveys the reason for the referral and includes VAs, IOPs and refraction, any relevant background information and an indication of priority, he said.
Cataract referrals for shorter wait times
Complete information is critical when referring for cataract to avoid longer wait times, said Kumar. The referral should include information on vision (RE unaided PH, LE unaided PH, binocular vision); ocular comorbidities (relevant, injuries, previous ocular surgery, family history, AMD, narrow angles, systemic comorbidities like diabetes); type of cataract (posterior or sub capsular opacities); quality of life questionnaire; and the Clinical Priority Assessment Criteria (CPAC) score. It is also a good idea to confirm with the patient that they want to have surgery prior to referral, said Kumar.
The national threshold for cataract surgery is 46 points. Optometrists registered with the New Zealand Association of Optometrists should be able to access the National Prioritisation Web Service to complete the CPAC scoring system (https://npi.1000minds.com/). However, if for some reason the referring optometrist cannot access it, the Counties team will complete the scoring as long as the relevant information is provided, Kumar said.
Paediatric optometrist Rebecca Findlay and orthoptist Grace Yung rounded off the evening covering Counties’ paediatric services and how to refer this cohort. Referrals should include information on VAs, refractive error (if present), onset of condition, which eye is involved, diplopia (if present), squints (direction, magnitude and motility defect), general health conditions or developmental delays and existing prescription. Any queries (no referrals) can be directed to kids.eyes@middlemore.co.nz.
As well as the Counties’ referral information, optometrist guests were served a healthy dose of CPD plus a tour of the premises. Chatting to some of the visitors afterwards, this was exactly what they came for. Well done, Counties.