Shingles: a crucial conversation for the over-50s
Since herpes zoster (HZ) infections can cause permanent vision loss, eyecare professionals should make it a priority to talk to patients aged over 50 years about the importance of preventing shingles through vaccination, said Dr Rachael Niederer, an ophthalmologist and senior lecturer at Auckland University.
Dr Niederer emphasised the importance of the Shingrix vaccine, which is administered in two doses, two to six weeks apart. This vaccine has shown remarkable efficacy, she said, with an overall effectiveness of 97.2% in individuals aged 50 and older, and 91.3% in those aged 70 and older. “Shingles is a terrible disease. About 1 in 10 people who get it will lose their vision. It's common and I frequently see people who lose their vision due to shingles,” she said.
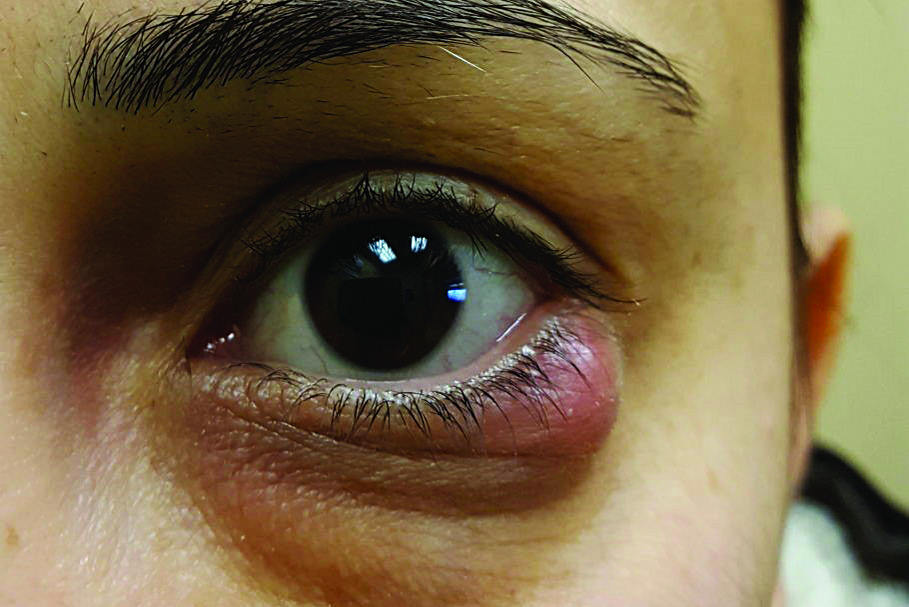
When the varicella-zoster virus reactivates in the ophthalmic division V1 of the trigeminal nerve, it can lead to herpes zoster ophthalmicus (HZO), which often manifests as conjunctivitis, uveitis and keratitis, she said. Approximately one in three people in New Zealand will experience shingles in their lifetime, with 10–15% of these cases affecting the V1 distribution and half of these involving the eye. The risk of moderate (6/15) permanent vision loss is 1 in 10, while severe (6/60 or worse) vision loss is 1 in 30 for those with V1-distribution.
Further HZO complications include corneal scar, neurotrophic keratopathy, band keratopathy, corneal melt, corneal perforation and acute retinal necrosis or panuveitis, all contributing to vision loss, she added.
Patients with shingles can suffer from permanent nerve pain, chronic dry eye, and even dementia, said Dr Niederer, with cranial nerve palsy leading to stroke and double vision in rare cased.
Recent evidence suggests shingles can have profound neurological effects, she said. “Strokes typically occur two to four months after infection, possibly due to inflammation of blood vessels caused by the virus. The risk of dementia persists for several years after a shingles episode.”
Dr Niederer said she is excited by the research in this area, citing a large meta-analysis in Neurology which concluded the herpes zoster vaccination was associated with a reduction of the risk of dementia.
A study in Nature Medicine also found subjects receiving Shingrix had a 17% lower risk of being diagnosed with dementia in the six years after inoculation, compared to people who got the Zostavax vaccine. Further, a GSK study of 600,000 patients showed those who got the Shingrix vaccine were about 23% less likely after five years to have a diagnosis of dementia, compared with people receiving Zostavax.
In New Zealand, only those aged 65 years or who are immunocompromised are eligible for the free vaccine; for others, immunisation costs between $600 to $800. “If you are 66, you don't get it funded, which is crazy!” said Dr Niederer.
Dr Niederer advised that patients must wait at least 12 months after their shingles episode (off treatment and no flare-ups) before receiving the vaccine.