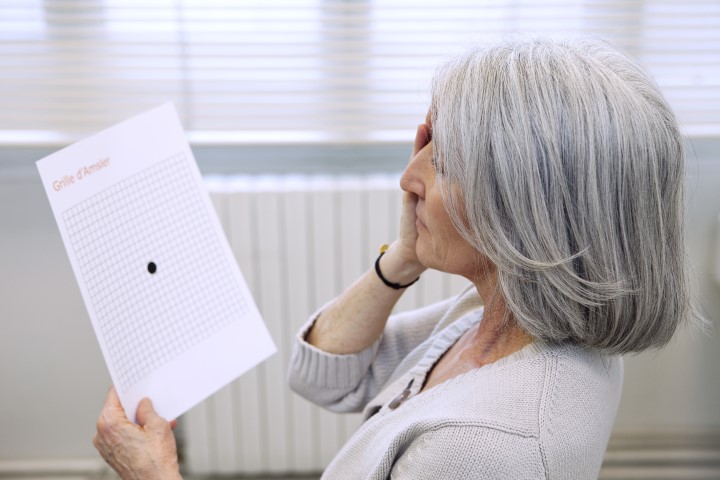
Support for non-medical ‘graders’ to screen for DMO
Trained, non-medical ‘graders’ used multimodal imaging to identify diabetic macular oedema (DMO) with 90% accuracy, revealed a new study.
The ‘Effectiveness of multimodal imaging for the evaluation of retinal oedema and new vessels in diabetic retinopathy’ (EMERALD) study was led by Professor Noemi Lois at Queen's University Belfast. Researchers said their findings support the call for more non-medical graders to help lower costs in taxpayer-funded healthcare systems by releasing ophthalmologists’ time, while increasing the DMO- and proliferative diabetic retinopathy (PDR)-monitoring capabilities of clinics in rural communities. While the potential to reduce waiting times could save more people’s sight, they said.
Graders in the study were trained to use spectral-domain optical coherence tomography (OCT) for DMO and 7-field Early Treatment Diabetic Retinopathy Study (ETDRS) and ultra-widefield (UWF) fundus images for PDR. While this pathway showed high sensitivity (90%) in detecting DMO, it was less effective in detecting PDR, albeit at a higher sensitivity than the 80% threshold set by researchers. Importantly, the sensitivity of the ophthalmic grader pathway to detect high-risk PDR – with preretinal or vitreous haemorrhage, or both – was higher (87%) when using UWF fundus images.
The level of specificity of ophthalmic graders detecting DMO and PDR (31% and 54%-60%, respectively) was not high, said researchers. Although this implies more false-positive patients who need to be seen by an ophthalmologist, even this specificity could lead to useful savings in ophthalmologists’ time, they said.
Retinal clinics are stretched because anti-VEGF agents are also used to treat other diseases, including age-related macular degeneration (AMD) and retinal vein occlusion, said researchers. “Cancellations of all routine appointments worldwide during the pandemic have exacerbated this problem to unprecedented levels. Thus, it is imperative that new ways to increase efficiency and capacity of ophthalmic clinics are identified and, if safe and acceptable, are implemented.”
The full study was published in Ophthalmology in April 2021.