Valacyclovir shows promise against HZO
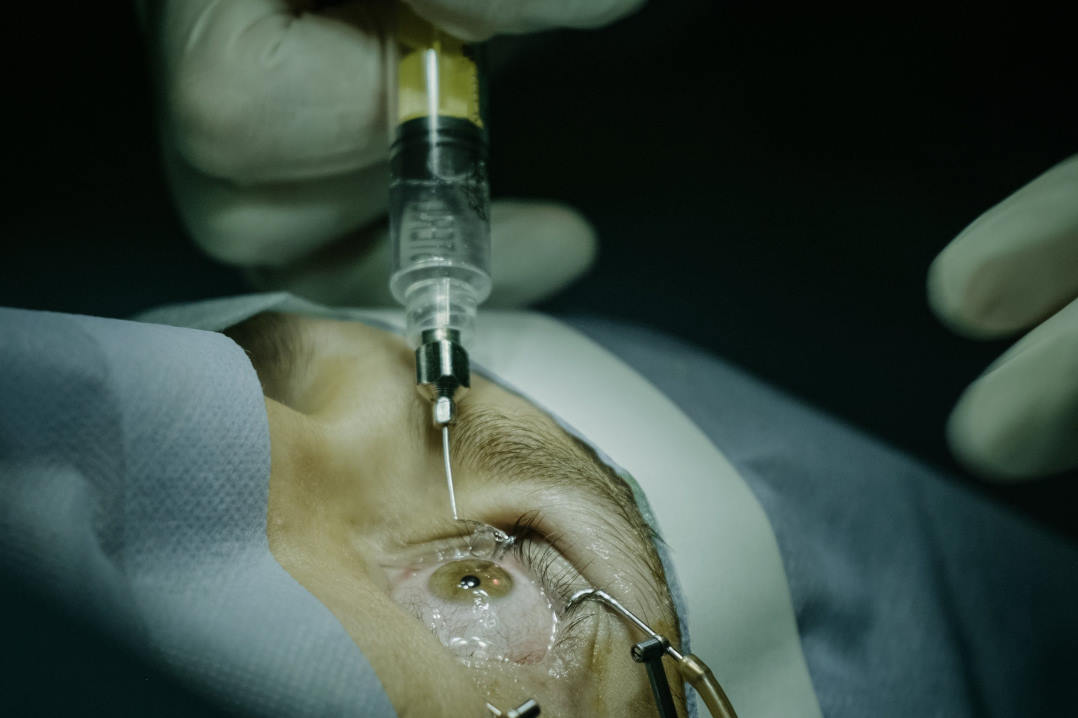
Auckland researchers, as part of a larger international study, have found that a year-long, low-dose course of valacyclovir can reduce recurrence and pain in herpes zoster ophthalmicus (HZO) patients.
The eight-year Zoster Eye Disease Study (ZEDS) enrolled over 500 participants with eye-affecting shingles and assessed the effectiveness of daily 1g valacyclovir over 12 months. Roughly half received valacyclovir, while the remainder received placebo.
In a news announcement from the University of Pennsylvania, study co-chair Professor Bennie Jeng, chair of ophthalmology at the university’s Perelman School of Medicine, said up until now, there had been no proven long-term treatment for new, worsening, or repeated episodes of shingles. “So the results of this study provide convincing evidence for using long-term, low-dose antiviral treatment.”
Study contributor Professor Elizabeth Cohen, from the NYU Grossman School of Medicine and NYU Langone Health – who designed the study after she was affected by shingles-related vision loss – reported valacyclovir reduced the risk of new or worsening eye disease by 26% within 18 months of treatment initiation. Patients on valacyclovir were also 30% less likely to experience multiple HZO flare-ups at a year or a year-and-a-half later, compared with those on a placebo, she said.
New Zealand-based ophthalmologists Drs Jay Meyer and Rachael Niederer, both of whom ran the University of Auckland’s ZEDS trial, said the results are “exciting news for our patients with HZO, as this treatment may reduce the overall burden of the disease”. They emphasised the study’s significance, since recurrences in HZO are common and contribute to long-term vision loss. “HZO causes eye involvement in 50‒80% of patients, with half requiring prolonged topical steroid treatment and permanent vision loss occurring in 10%,” said Dr Niederer.
Another ZEDS finding was that the treatment group required less pain relief medication at the end of the study. “Post-herpetic neuralgia is a chronic nerve pain condition that can follow a shingles outbreak and can be difficult to treat, with a major impact on quality of life. The results of this trial support the use of a year of prophylactic valacyclovir for patients with HZO associated with keratitis or uveitis, as well as for patients with HZO requiring pain relief medication such as gabapentin,” said Dr Neiderer.
Looking ahead, Prof Jeng said the ZEDS team aims to investigate whether extended antiviral treatment prevents complications like glaucoma and scleritis and will explore the effects of shingles vaccination on study participants, including its impact on Covid-19 outcomes.
Funded by the National Institutes of Health, ZEDS was conducted across 95 medical centres in the US, Canada and New Zealand. Its findings were presented in October at the Cornea and Eye Banking Forum and the American Academy of Ophthalmology’s annual meeting.