An ultra-widefield view of retinal pathologies
Retina Specialists’ 2023 winter seminar proved a warm respite from the blustery, wet and cold Auckland weather. With a unique approach, which challenged the audience to match the Retina Specialists team’s diagnostic skills across a series of case studies using an interactive app, the oversubscribed evening included some fascinating cases where the obvious answer was not always the correct one.
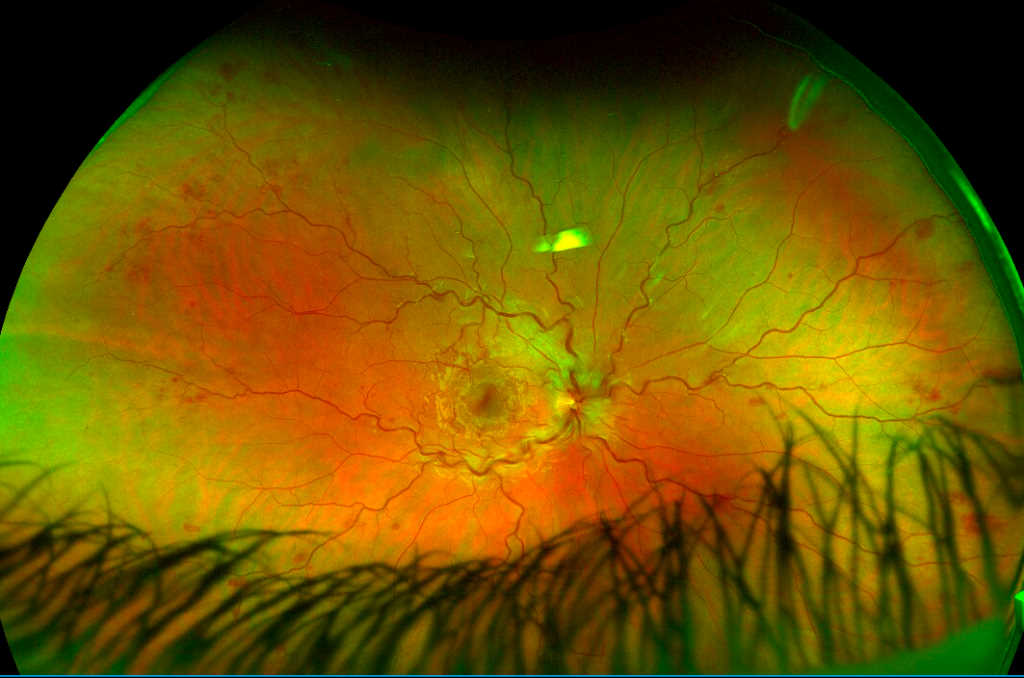
First up, Dr Rachel Barnes shared some interesting cases of sickle cell retinopathy, where blocked blood vessels in the choroid and the retina result in abnormal vessel growth and retinal thinning. Ocular features include peripheral ‘sea fan’ neovascularisation, salmon patch haemorrhages, starbursts and angioid streaks.

Shirley Chang and Dr Rachel Barnes
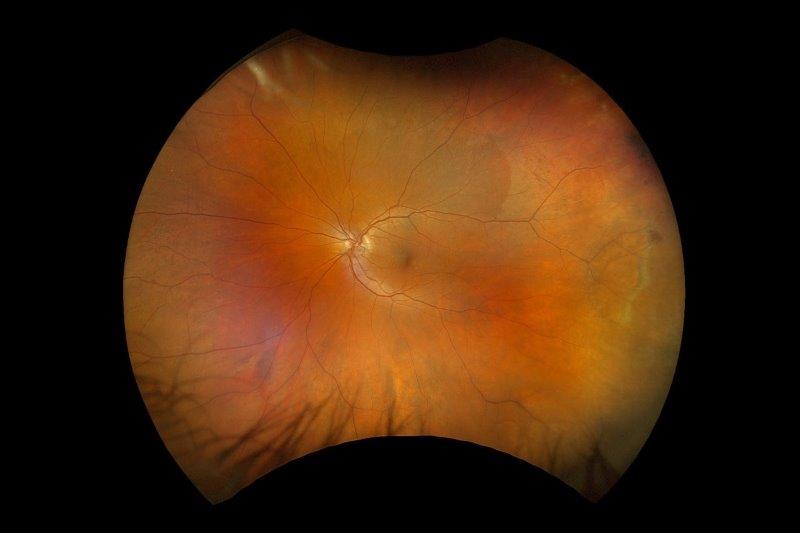
Sticking with the theme of new, abnormal vessel growth in the periphery as a genetic disease marker (while also demonstrating the usefulness of the team’s Optos ultra-widefield imaging technology), Dr Barnes’ next case focused on familial exudative vitreoretinopathy (FEVR), a relatively rare inherited disorder. FEVR’s inheritance patterns are autosomal dominant (AD), autosomal recessive and X-linked recessive, with AD being the most common and involving many different genes. It looks similar to retinopathy of prematurity and, like sickle cell retinopathy, it’s important to screen other family members when a patient is identified, said Dr Barnes.
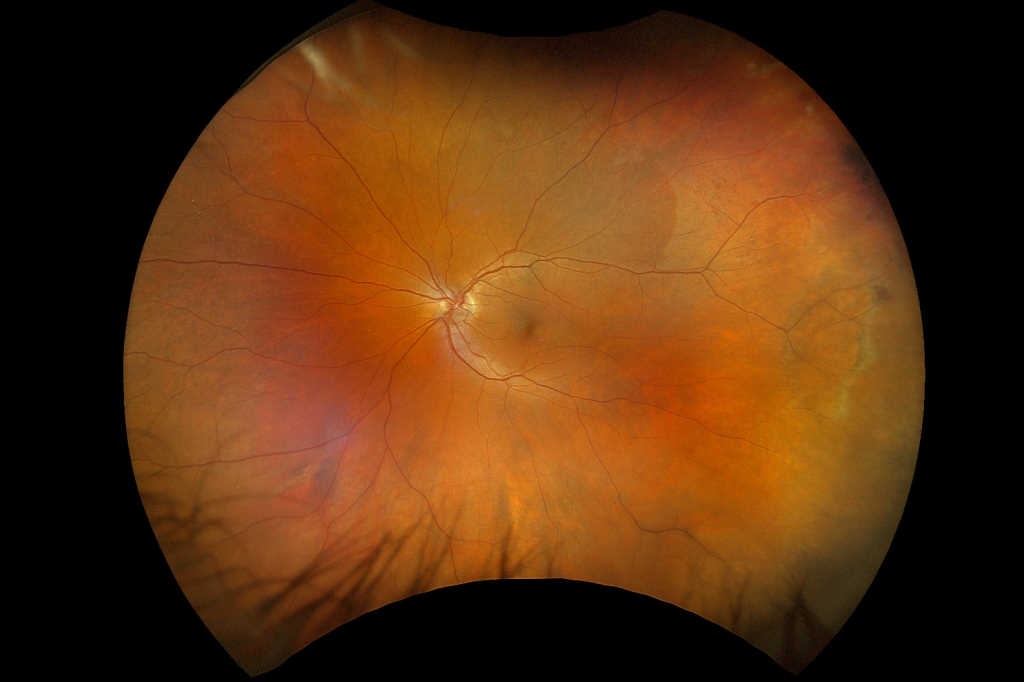
Associate Professor Andrea Vincent then put the audience through its paces with some more Optos-derived case images of torpedo maculopathy in a patient whose father had haemochromatosis, peripheral exudative and haemorrhagic chorioretinopathy (PEHCR) and a tricky CHRPE (congenital hypertrophy of the retinal pigmented epithelium) case.
Haemochromatosis, an inherited condition where the body’s iron levels build up over years, is very common in people with Scottish ancestry, said A/Prof Vincent. In the eye it can lead to non-arteritic posterior ischaemic optic neuropathy, conjunctival pigmentation, corneal iron deposits and microaneurysms along the main retinal vessels, plus retinal haemorrhages, similar to diabetic retinopathy.

Ran Jing and Dian Zhuang
A relatively rare condition, PEHCR is sometimes referred to as peripheral age-related retinal degeneration. It affects elderly patients and can mimic other conditions, including choroidal melanoma. Management includes observation, vitrectomy, anti-VEGF injections, laser and cryotherapy (though this can lead to retinal haemorrhages). Most PEHCR cases stabilise or regress with subretinal fibrosis, retinal pigment epithelium hyperplasia or atrophy, said A/Prof Vincent.
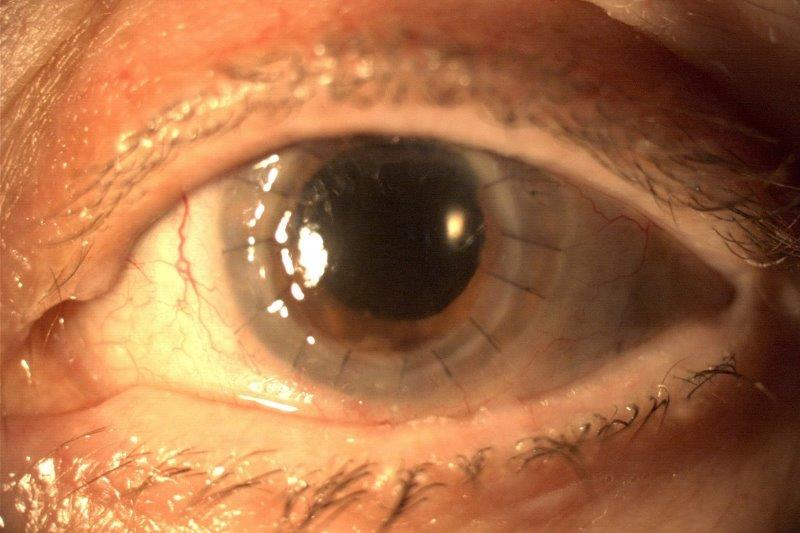
The evening’s host and closing speaker Dr Leo Sheck then took the audience on an amusing journey with a tricky cataract patient who had a high risk of vasculitis and cystoid macular oedema but was impatient to go on holiday to Malaysia. Challenging the audience with a couple of treatment options he’d faced, Dr Sheck reported that after a bit of tooing and froing, treatment discussion and a lot of trust, the patient was able to be treated, go on holiday, return and be treated again. As a result, they can still read and drive and have booked their next holiday to Antarctica! Key to the successful outcome in this case was being able to call on the other Retina Specialists team members’ skills, said Dr Sheck.
Again demonstrating the importance of ultra-widefield imaging and careful image assessment in some cases, Dr Sheck then discussed an interesting floater case, where the patient had left central retinal artery occlusion with cilioretinal artery sparing. If someone’s over 50, the most likely cause is an embolus in the neck, he said, while for younger people it’s likely to be structural heart disease, such as patent foramen ovale – a hole between the left and right upper chambers of the heart, which failed to close at birth and the patient is often unaware of. After a couple of brief quiz questions focusing on other, unrelated cases, Dr Sheck brought the evening to a close, leaving everyone looking forward to next year’s CPD-fuelled quiz evening.